Oligometastatic prostate cancer: outcomes and toxicity of stereotactic body radiation therapy (SBRT)
Elias Gomis Selles,
Spain
PO-1573
Abstract
Oligometastatic prostate cancer: outcomes and toxicity of stereotactic body radiation therapy (SBRT)
Authors: Elias Gomis Selles1, Óscar Muñoz Muñoz1, Patricia Cabrera Roldán1, Blas David Delgado León1, José Luis López Guerra1
1Virgen del Rocio University Hospital, Radiation Oncology, Sevilla, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
SBRT is a method of external beam radiotherapy (EBRT) that precisely delivers a high irradiation dose to a target in one or few treatment fractions. These characteristics make it a logical choice for metastasis-directed therapy in prostate cancer.
The main endpoint of this analysis is to assess the impact of this strategy on disease control. The secondary objective is to evaluate the toxicity of SBRT.
Material and Methods
Retrospective cohort study selecting patients with oligometastatic prostate cancer who received SBRT for metastases in a single institution between 2017 and 2022.
Data is analyzed using the Wilcoxon test and Cox regression. The Shapiro-Wilk test is used to study normality. We consider a significant result if p-value < 0.05.
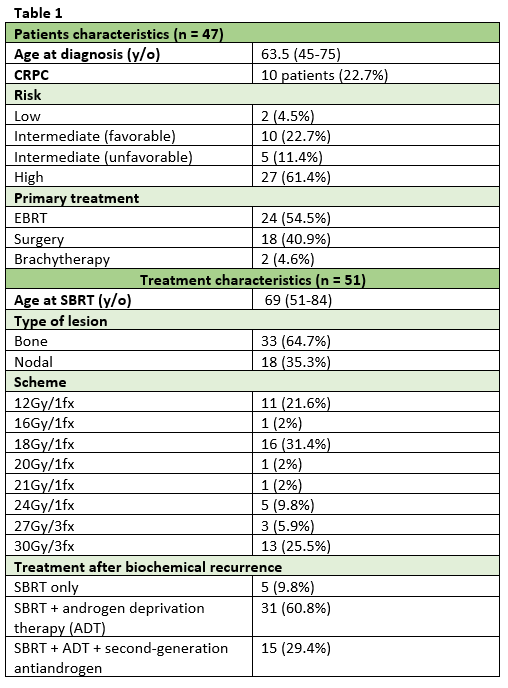
Forty-seven patients, representing a total of 51 metastatic lesions were selected (Table 1). The median follow-up period was 90 months from diagnosis (interquartile range, IQR, 74) and 15 months from SBRT (IQR 29). It was delivered between 1 to 3 fractions with a dose between 12 to 30Gy.
Results
The main location where SBRT was performed was bone (n = 33) followed by adenopathy (n = 18). Regarding the dose, the most used was the scheme of 18Gy in a single fraction (n = 16) followed by 30Gy in 3 fractions (n = 13).
Two patients (4.3%) developed local progression with a median of 5.50 months. Distant progression occurred in 9 patients (20.5%) with a median of 4 months. 71.4% of lesions presented a radiological response after SBRT. 2 deaths occurred, and none of them were related to prostate cancer. An increased risk of disease progression after SBRT was found in patients who developed castration-resistant prostate cancer (CRPC): HR 16.44, CI95% [3.48; 77.67]; p-value < 0.001. Ten patients (22.7%) developed biochemical progression after SBRT, with a median of 4 months. Two deaths occurred during the follow-up period, neither of which was related to prostate cancer.
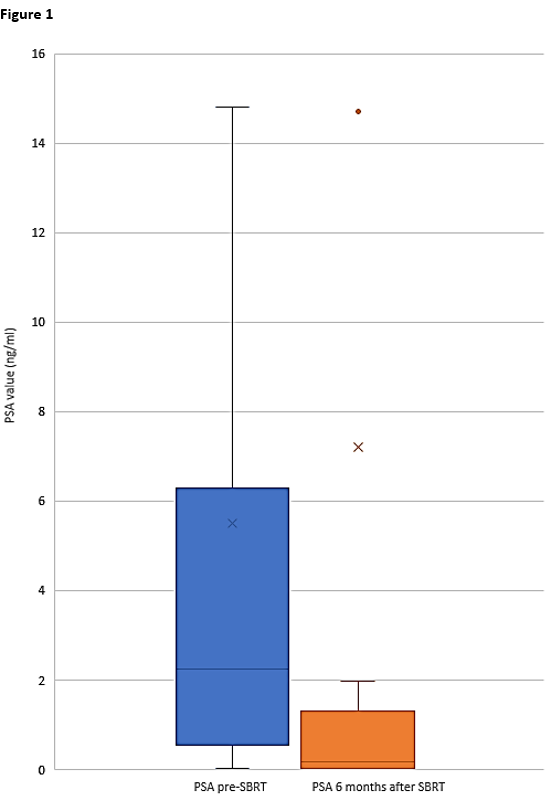
A significant drop in the PSA value after 6 months of treatment was identified (2.20ng/ml vs 0.25ng/ml, p-value 0.014) (Figure 1).
Eight patients presented acute toxicity (mild pain in all cases). Four patients (9%) developed chronic toxicity: 3 mild pain and 1 rectovesical fistula. Any patient presented a grade 4 toxicity neither needed to stop the treatment.
Conclusion
SBRT is a considerable option for oligometastatic patients due to its excellent local and biochemical control with a negligible toxicity profile. The rate of distant progression means that the role of SBRT must be reassessed with the aim of delaying systemic therapy or as part of a combination treatment.