Radiation-induced lymphopenia in pediatric high-risk neuroblastoma
Elias Gomis Selles,
Spain
PO-1569
Abstract
Radiation-induced lymphopenia in pediatric high-risk neuroblastoma
Authors: Elias Gomis Selles1, Óscar Muñoz Muñoz1, Blas David Delgado León1, Patricia Cabrera Roldán1, Ana María Burgueño Caballero1, José Luis López Guerra1
1Virgen del Rocio University Hospital, Radiation Oncology, Sevilla, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
The main objective of this study is to assess the impact of radiation therapy (RT) on hematological function in high-risk neuroblastoma pediatric patients and analyzed its relation with overall survival.
Material and Methods
Retrospective cohort study selecting all pediatric patients with adrenal high-risk neuroblastoma treated with radical intention with RT from October 2008 until august 2021. A comparison of bloodlines recount prior to RT, at a month over RT, and at the end of follow-up was performed and related to overall survival.
Results
Forty-two children with a median age of 3.24 years at diagnosis and 4.24 years of follow-up were selected.
We found a significant decrease in the recount of lymphocytes at a month over RT (median 1.28*103 cell/ml vs 0.84*103 cell/ml; p-value < 0.001). No significant increase was observed in any bloodline. We grouped the patients according to whether more than 73 days had elapsed from the transplant to the treatment (median for this interval) or if they were older or younger than 4 years (median age), without finding significant differences in the grade of lymphopenia post-RT.
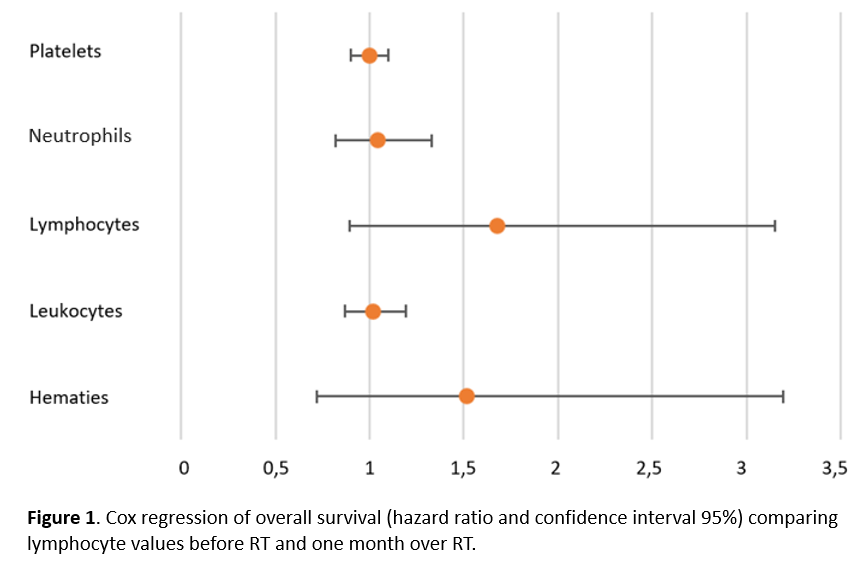
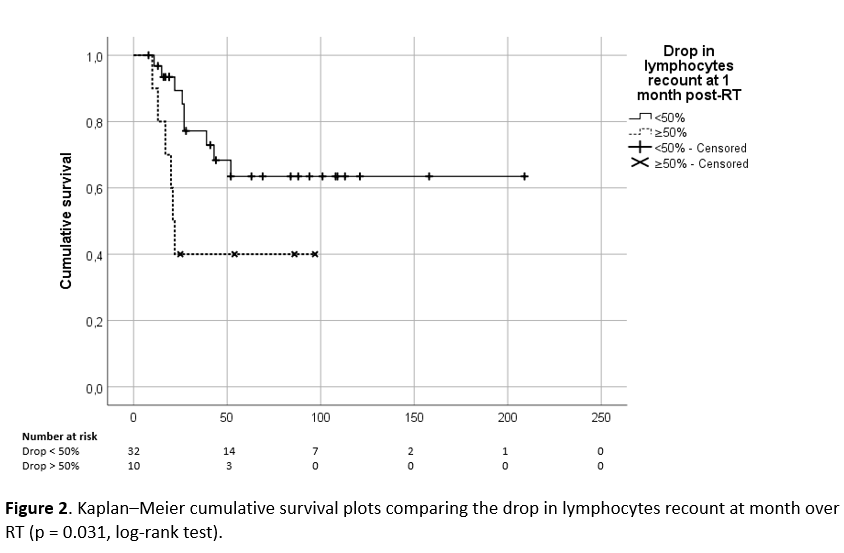
The survival analysis revealed an association of near significance between risk of death (overall survival) and acute drop in lymphocyte recount at one-month post-RT (HR = 1.68; p-value = 0.10; CI95% [0.894; 3.151])(Figure 1). For patients who experimented a drop in lymphocytes higher than 50% (n =10) of the previous value, we found a significant increase in risk of death during follow-up (HR = 2.97; p-value = 0.04; CI95% [1.046; 8.432]) (Figure 2). Six deaths occurred in this group, they were related in 5 cases in the context of relapse (3 of them in less than 120 after RT) and another was due to pulmonary edema and acute respiratory failure during infusion of anti-GD2 (antiganglioside type 2). Moreover, this group of patients presented more relapses during or after immunotherapy too (80% vs 43%; odds ratio = 1.82; p = 0.045; CI95% [1.109; 3.012]).
At the end of the follow-up, it was appreciated a significant increase in all bloodlines except in hemoglobin.
Conclusion
Our data suggest that these patients experiment a significant acute decrease in lymphocytes after RT which could impact in the prognosis. A drop higher than 50% of previous lymphocyte values is related to a significant decrease in overall survival. In accordance with long-term analysis, all bloodlines were in the physiological range. Our study is limited by a relatively small sample , a long observation period, and the presence of different RT techniques. Future studies should aim for a prospective and multicenter analysis of toxicities and therapeutic strategies in these patients.