Local control rates after MR-guided single fraction SABR for lung tumors
Hilâl Tekatli,
The Netherlands
PO-1331
Abstract
Local control rates after MR-guided single fraction SABR for lung tumors
Authors: Hilâl Tekatli1, Miguel Palacios1, Famke Schneiders1, Niels Haasbeek1, Frank Lagerwaard1, Suresh Senan1
1Amsterdam UMC, Radiation Oncology, Amsterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Single fraction (SF) stereotactic radiotherapy (SABR) is an effective treatment in patients with peripheral lung tumors. Most published experience with SF-SABR has been using CT-based treatment planning, with often on-couch cone-beam CT guidance. MR guided adaptive radiotherapy is a recent development, and there are concerns about the accuracy of target definition, treatment planning and MR-guided SABR delivery. We report on clinical outcomes following MR guided SF-SABR for lung tumors.
Material and Methods
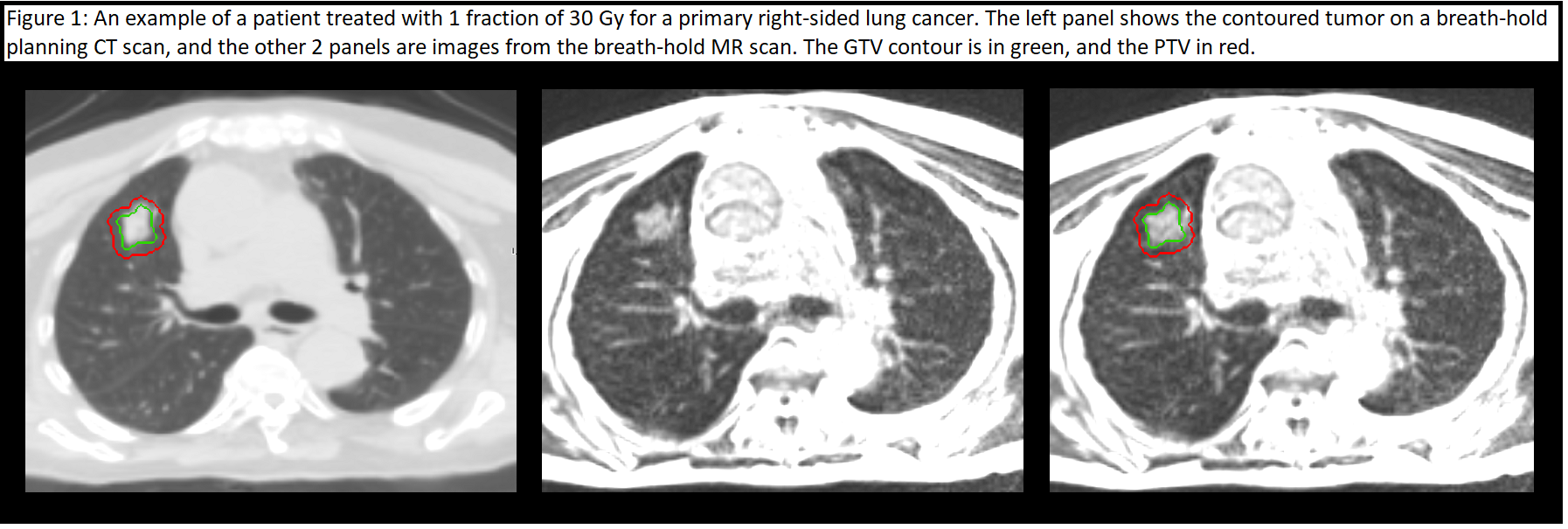
Details of patients with peripheral lung tumors undergoing MR guided SF-SABR at a single institution since 2018 were accessed from a prospective institutional database. This study was approved by our Medical Ethics Review Committee. Treatment simulation is performed using a 17-s breath-hold 3D MR based on a true FISP sequence acquisition on a 0.35 T MR scanner. Tracking performance was assessed visually during MR simulation. GTV contouring was first performed on a breath-hold planning CT scan, followed by contours on a rigid co-registered 3D MR scan by the same clinician. Any discrepancies in GTV’s between imaging techniques were reviewed by a second clinician to reach a consensus. SABR plans were generated using step-and-shoot IMRT beams, and normalized to cover 95% of the PTV by the prescription dose. A PTV Dmax of up to 140% was used. On-table contour editing was performed if considered clinically relevant. A 5 mm PTV margin, and a 3 mm gating window, were used. SABR was delivered using automatic beam gating during repeated breath-holds, and under continuous visualization of the tracked GTV in a sagittal MR plane.
Results
A total of 51 consecutive patients were treated between 2018 and 2022. The majority (69%) had a primary NSCLC. One patient was treated for two tumors in the same lobe. Median PTV was 11.2 cc (range 3.9-53.5). The SF dose was 20 Gy (2%), 24 Gy (4%), 28 Gy (4%), 30 Gy (31%) or 34 Gy (59%). Details of treatment duration were available for 38 patients and measured from the patient entered the changing room to the end of delivery. Median duration for the period 2018-2020 was 119 minutes (range 65-178), and 90 minutes (range 60-192) for the period 2021-2022. After a median follow-up of 18.7 months (95% CI 14.8-22.5), 2-year OS was 81%, ranging from 89% for primary lung tumors to 60% for metastases. All but 4 patients were eligible for assessment of local control. Local recurrences occurred in 2 patients (4%), manifesting at 9.4 months and 37.3 months post-SABR, respectively. Acute toxicity within 90 days post-SABR was observed in 2 patients (1 patient with grade 2 radiation pneumonitis and 1 with severe temporary back pain due to the duration of SABR delivery).
Conclusion
The early results of MR guided SF-SABR delivered in breath-hold reveal high tumor control rates, indicating that the use of automatic beam gating with a 3 mm gating boundary is safe for patients with peripheral lung tumors.