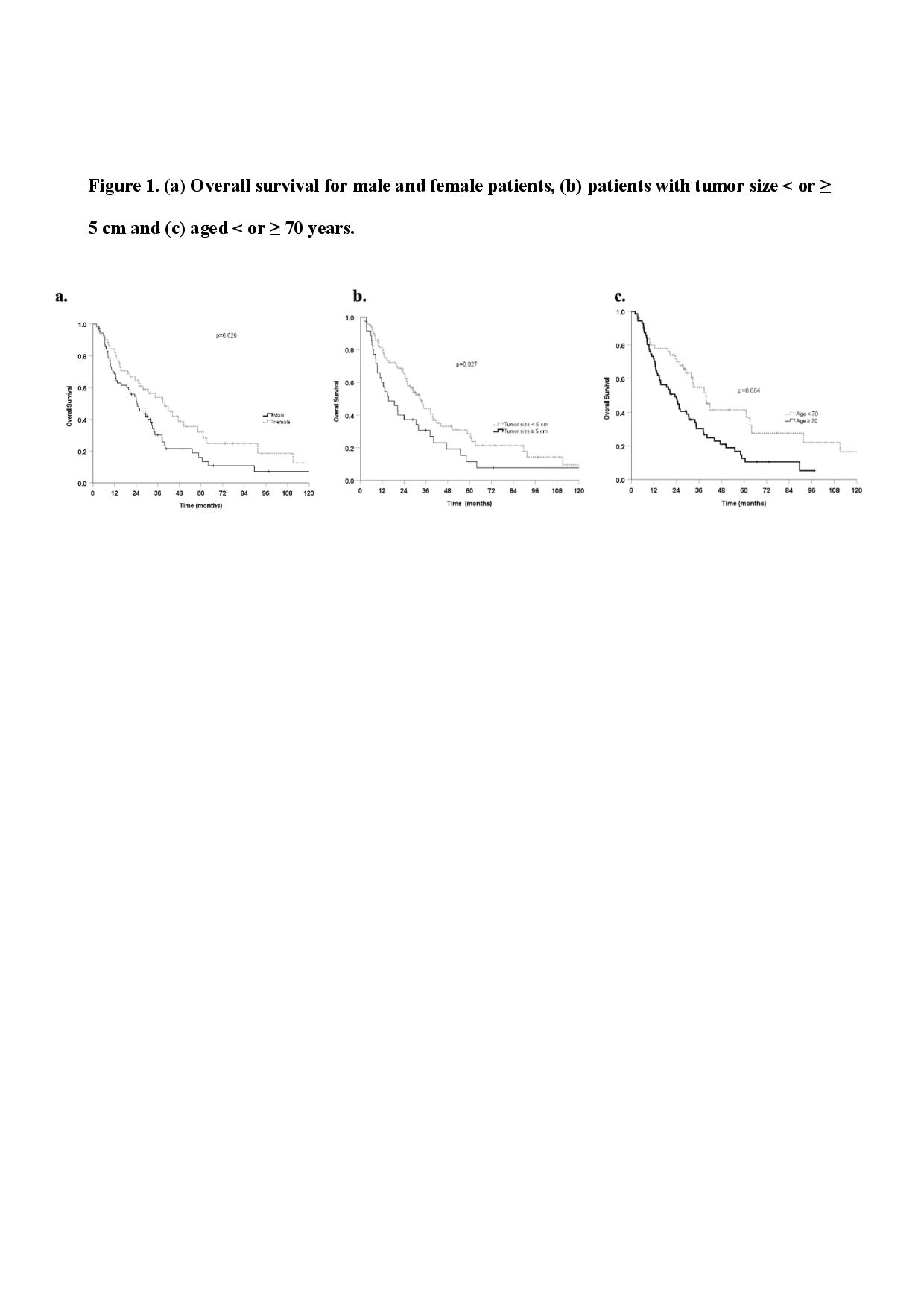
A total number of 126 UC lung tumors were reviewed. Table 1 summarizes the patient, treatment and tumor characteristics. Median follow-up time was 23 months. Median OS was 29.3 months (95% CI 22.4-36.21). The 1-, 2- and 5- year OS rates were 75%, 58% and 23%, respectively. PFS and LC rates at 1 ,2 and 5 years rates were 63%, 41% and 15% (median 16 months, 95% CI 8.9-23.1) and 86%, 78% and 61%, respectively. Female gender (HR, 0.61 95% CI, 0.4-0.9, p 0.027) were significantly associated with better OS (Figure 1) and age ≥ 70 years (HR 1.91, 95% CI 1.2-3.0, p 0.005) and tumor ≥ 5 cm (HR 1.64, 95% CI 1.1-2.5, p 0.028) correlated with worse OS (Figure 1) at univariate analysis. A borderline detrimental association (p 0.07) between OS and tumor-trachea distance > 5 mm was also found. In the multivariate analysis female gender (HR 0.6 95% 0.4-1.0, p 0.05), age ≥ 70 years (HR 1.9 95% CI 1.2-3.0, p 0.006) and tumor-trachea distance > 5 mm (HR 2.2 95% CI 1.2-4.2, p 0.015) resulted as independent factors significantly associated with OS. The patients treated for primary tumors showed a significantly better PFS at Kaplan-Meier analysis (p < 0.001). The median PFS was 26.2 months (95%CI 0.5-52.0) and 12.4 months (95% CI 7.3-17.5) for group of primary tumor and oligometastases, respectively. Kaplan-Meier curves showed a positive trend for tumor < 5 cm and PFS (p 0.068). Moreover, in the subset of patients with primary lung cancer, tumor < 5 cm was correlated with a significantly better PFS (p 0.004). The acute G2 dysphagia, cough and dyspnea were 11%, 5% and 3%, respectively. Acute G3 dyspnea was experienced by one patient. Late G3 toxicity was reported in 4% of the patients, consisting of pain and dyspnea in 4 and 1 patients, respectively.