Implementation of daily online adaptive radiotherapy for post-operative whole breast irradiation
Koen Nelissen,
The Netherlands
PO-1293
Abstract
Implementation of daily online adaptive radiotherapy for post-operative whole breast irradiation
Authors: Koen Nelissen1,2, Wilko Verbakel1,2, Barbara Rijksen1, Marjan Admiraal1, Jessica van der Himst1, Ewa Bucko1, Ben Slotman1,2, Desirée van den Bongard1,2,3
1Amsterdam UMC location Vrije Universiteit Amsterdam, Radiation Oncology, Amsterdam, The Netherlands; 2Cancer Center Amsterdam, Cancer Treatment and Quality of Life, Amsterdam, The Netherlands; 3Cancer Center Amsterdam, Cancer Biology and Immunology, Amsterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
During postoperative whole breast irradiation (WBI), unexpected dosimetric deviations can occur due to breast contour changes resulting from resorption of breast seroma/hematoma, oedema either postoperatively or during WBI, or arm/body positioning variation. In 10-15% of cases, repositioning after setup imaging is not sufficient, and offline plan adaptation is required. This results in 2-3 days delay in continuation of WBI. Daily online adaptive radiotherapy (OART) provides the opportunity to adapt for contour changes during treatment. Our aim is to evaluate the implementation of OART in post-operative WBI.
Material and Methods
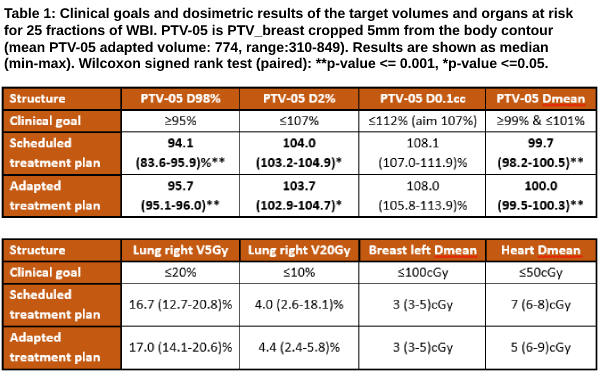
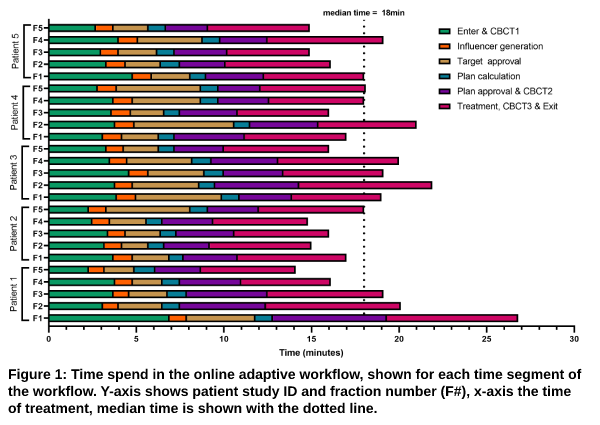
The BREAST-ART study (IRB2021.0624) is a single-arm prospective trial. All patients with right-sided breast cancer referred for WBI after BCS were eligible. First, robust templates were developed for offline and online treatment planning to a total dose of 26Gy in 5 fractions with a four beam IMRT tangential beam setup. CTV breast was expanded by 5mm to PTV breast, both were cropped 5mm from the body contour. Clinical goals used in the template to create the reference treatment plan (TPR). are shown in Table 1. During the OART procedure, the influencer structures (i.e. used in target propagation) and targets were reviewed by radiotherapy technologists (RTTs) and approved by a radiation oncologist (RO). Adapted treatment plan (TPA) was evaluated by the RTTs, RO, and medical physicist before treatment. Patient experience was evaluated using in-house developed questionnaires after sessions one and five, scoring treatment satisfaction on a 4-point Likert scale. Dosimetric, DICOM images and time data was exported from the clinical systems. The Wilcoxon signed rank test was used to evaluate differences between scheduled (=TPR calculated on daily anatomy) treatment plan (TPS) and TPA. Acute toxicity was evaluated according to Common Toxicity Criteria V5.0 at baseline after WBI(n=5) up to 3 months after WBI(n=2).
Results
We obtained signed informed consent of five right-sided breast patients with post-operative WBI. Two patients were treated with standard skin marks for positioning, for three patients less (n=2) or no(n=1) marks were used. Patient experience scores were 3-4, median time needed for the adaptive treatment was 18.0(range:14-27)min (Figure 1). Dosimetric results of the target volumes and organs at risk are shown in Table 1. For all patients TPA was used. Influencer structures were adapted during 11, and target structures during 7 fractions. Median CTV volume increased with 4.1(-3.3 to 14)% compared to the initial volume on the planning CT. Only grade 0-1 acute toxicity was observed.
Conclusion
OART for right-sided WBI is feasible and safe within an acceptable time per fraction, including good patient comfort within the clinical dosimetric requirements. Positioning using marks/tattoos could be omitted in future OART patients. We will expand this study for more complicated breast indications such as locoregional radiotherapy.