Extended reality as a novel opportunity to unleash the power of radiotherapy in the digital era
Federico Mastroleo,
Italy
PO-1105
Abstract
Extended reality as a novel opportunity to unleash the power of radiotherapy in the digital era
Authors: Federico Mastroleo1, Giulia Marvaso2, Matteo Pepa1, Stefania Volpe1, Mattia Zaffaroni1, Maria Giulia Vincini1, Giulia Corrao1, Luca Bergamaschi1, Ketti Mazzocco3, Gabriella Pravettoni3, Roberto Orecchia1, Barbara Alicja Jereczek-Fossa1
1IEO, Radiation Oncology, Milan, Italy; 2IEO, Radiation Oncology, Milano, Italy; 3IEO, Psycho-Oncology, Milan, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
The aim of the work is to provide a glance at the recent developments in extended reality (XR), in particular virtual reality (VR) and augmented reality (AR), to support students’ education, personnel training and patients’ empowerment in radiation oncology.
Material and Methods
A literature search was performed to find articles written in English, dating from 1995 to 2022, and on the use of XR for educational use at the medical student level, for radiation oncology professionals and for patients’ education in RT field. A total of 1012 records were considered for study inclusion, of which 41 papers were deemed eligible. PRISMA extension for scoping review has been adopted.
Results
Our work clearly shows that such technologies have already become a reality in many radiation-oncology-dealing-institutions worldwide and they represent an effective strategy for raising educational standards, improving health workers’ skills and promoting patients’ well-being and compliance. In the educational context, XR could broaden the chances for radiation oncology to better engage students with hands-on experience and to improve both their learning experience and their clinical skills. In brachiterapy, a realistic training VR scenario is able to provide an immersive experience, helping doctors to become familiar with the surgery scene and with the location of the source, increasing placement accuracy and confidence of the operator, and thus the rate of success. On the patients’ side, it could foster their empowerment in RT, with the intent of alleviating psychological distress, promoting awareness, and, ultimately, enhancing compliance and oncological outcomes. XR could help in hypnosis guidance, helping the control of the respiratory motion with beneficial effects on patient’s positioning stability during treatment.
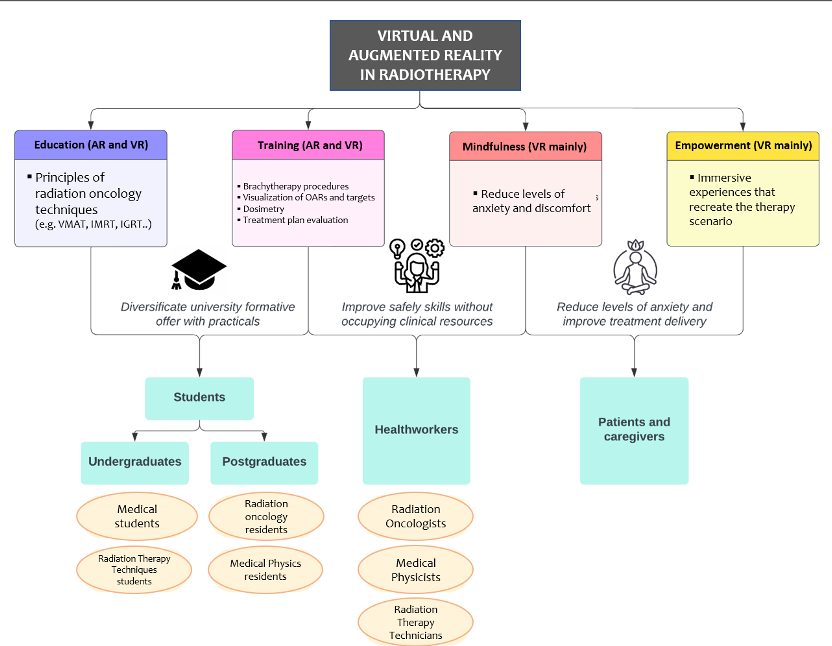
Conclusion
XR technologies could be valid instruments for promoting awareness of radiation oncology as a discipline with its own identity and respect in the scientific community. Their further implementation and development could be the potential driving force of a much hoped-for revolution in the way patients are treated and radiation oncology is taught.