Multicentre validation of the signal fading model of a new OSL film dosimeter
Laurence Delombaerde,
Belgium
MO-0309
Abstract
Multicentre validation of the signal fading model of a new OSL film dosimeter
Authors: Laurence Delombaerde1, Marco Caprioli1, Miriam Both2, Leonie Michielsen2, Erwann Rault3, Ileana Silvestre Patallo4, Alexandros Douralis4, Ilias Billas4, Mohammad Hussein4, Paul Leblans5, Dirk Vandenbroucke5, Christianus M.A. Leenders5, Wouter Crijns6
1UZ Leuven, Department of Radiotherapy-Oncology, Leuven, Belgium; 2Erasmus MC, Radiotherapy, Rotterdam, The Netherlands; 3Centre Oscar Lambret, Radiothérapie, Lille, France; 4National Physical Laboratory, Medical Radiation Physics, London, United Kingdom; 5Agfa NV, Innovation Office, Mortsel, Belgium; 6UZ Leuven, Department of Radiation-Oncology, Leuven, Belgium
Show Affiliations
Hide Affiliations
Purpose or Objective
Optically Stimulated Luminescence (OSL) film dosimeters display signal fading following irradiation due to spontaneous recombination of energetically unstable electron-hole traps. A power-law signal fading model for a new type of OSL film dosimeter was developed by Caprioli et al. (article accepted for publication). In this study we performed a multicentre validation of the model under different irradiation conditions.
Material and Methods
Protocol: A measurement protocol was distributed to 3 participating centres containing a description of the measurement setup, the irradiation and read-out conditions. Participating centres had received a BaFBr:Eu2+ based OSL film, prior to onset of this study within the QUARTEL project (see Conflict-of-Interest). After irradiation the films were digitized (adjusted scanner model CR-15X, Agfa NV) by the participating centre. Digital images were collected and processed by the organizing centre.
Measurements: Films were placed below 10 cm of solid water with SSD 90 cm and at least 10 cm of backscatter material. A total of 12 irradiations were performed by every centre with irradiation times (t_ir) between 2 and 20 mins and scanning times (t_scan) from 5 to 60 mins after onset of the delivery. Participants were free to select the delivered dose and dose rate, but were advised to cover a clinical range (2 – 30 Gy). A region-of-interest (ROI) of 1x1cm² at the centre of the delivered field was used to calculate the mean signal. The linear fading model from Caprioli et al. is the following:
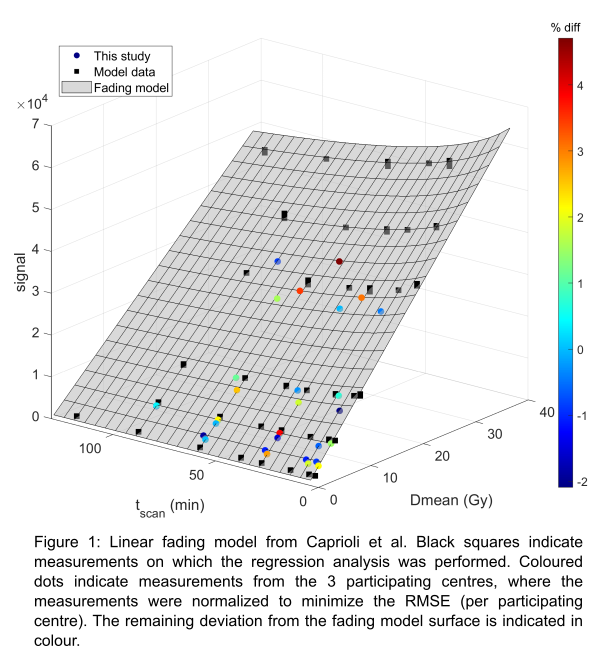
S(Dr_m,t_ir,t_scan)=A x Dr_m x t_ir x(t_scan+ τ)^(-n)
where the signal (S) is dependent on the dose rate Dr_m, t_ir and t_scan with A the sensitivity, τ and n OSL material specific parameters. For model validation the fading specific parameter (τ and n) were kept constant. Only the parameter A was adjusted to account for a global sensitivity variation that can be expected for the different setups. A was scaled by the mean deviation per treatment site (12 measurements) to the original model by Caprioli et al. The resulting deviations from the fading model were extracted by calculating the residual RMSE.
Results
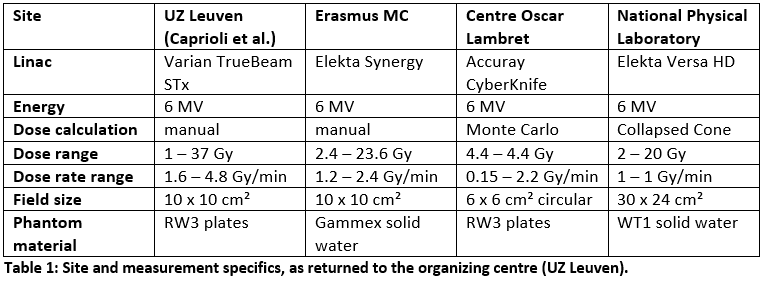
A total of 36 measurements were collected from three sites, which had different linacs and used different field sizes as indicated in table 1. All sites used a 6MV photon beam and scanned the films at a resolution of 100x100 µm². Following normalizations were required: +3.6%, -9.2% and +10.6%. Figure 1 shows the data after normalization. The median dose difference was 0.33 % (range: -2.1% to 4.7%). 75% of the validation measurements (27/36) were within 2% of the fading surface.
Conclusion
The linear fading model of Caprioli et al. accurately models the fading behaviour of the BaFBr:Eu2+ OSL-type dosimeter. Due to the sensitivity of the OSL signal to the field size, film production, energy spectrum and scanner settings a normalization was required per centre. A site specific signal-to-dose calibration protocol will therefore be required.