Analysis of Performance and Motion Management Technique of the IROC Thoracic Phantom
MO-0305
Abstract
Analysis of Performance and Motion Management Technique of the IROC Thoracic Phantom
Authors: Hunter Mehrens1, Vanessa Panettieri2, Stephen Kry1
1MD Anderson Cancer Center, Radiation Physics, Houston, USA; 2The Alfred Hospital, Alfred Health Radiation Oncology, Melbourne, Australia
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiotherapy facilities participating in national clinical trials in the United States must successfully irradiate credentialing phantoms from the Imaging and Radiation Oncology Core (IROC). This work analyzes the relationship between motion management technique and phantom performance for IROC’s thoracic phantom.
Material and Methods
IROC’s thoracic phantom contains an oblong spheroid primary target made of solid water encased by cork. The accuracy of the delivered dose in the primary target is assessed using thermoluminescent dosimeters (TLDs) and three planes of GAFchromic film. The phantom is placed on an acrylic motion platform that provides 2cm of sinusoidal motion in the superior-inferior direction. Results of 1,643 phantom irradiations between 2012-2020 were retrospectively analyzed. In addition, superior-inferior extent of the TPS’s 90% isodose line was measured. We evaluated the relationship between motion management technique and pass rate of the phantom using univariate analysis. Tumor control probability (TCP) was calculated for a subset of 279 irradiations using BioSuite v12.01. TCP was calculated using the Marsden Poisson model.
Results
The overall average pass rate of the phantom was 86.6%. Motion management technique had a significant impact on phantom pass rate (p < 0.001), as gating had a lower pass rate compared to tracking and static (p < 0.03) and ITV had a lower pass rate compared to static (p = 0.018). The extent of coverage (superior-inferior) was significantly different based on motion management technique (p <0.001). All techniques provided equivalent TCP. Surprisingly, as superior-inferior extent increased, the pass rate of the phantom decreased.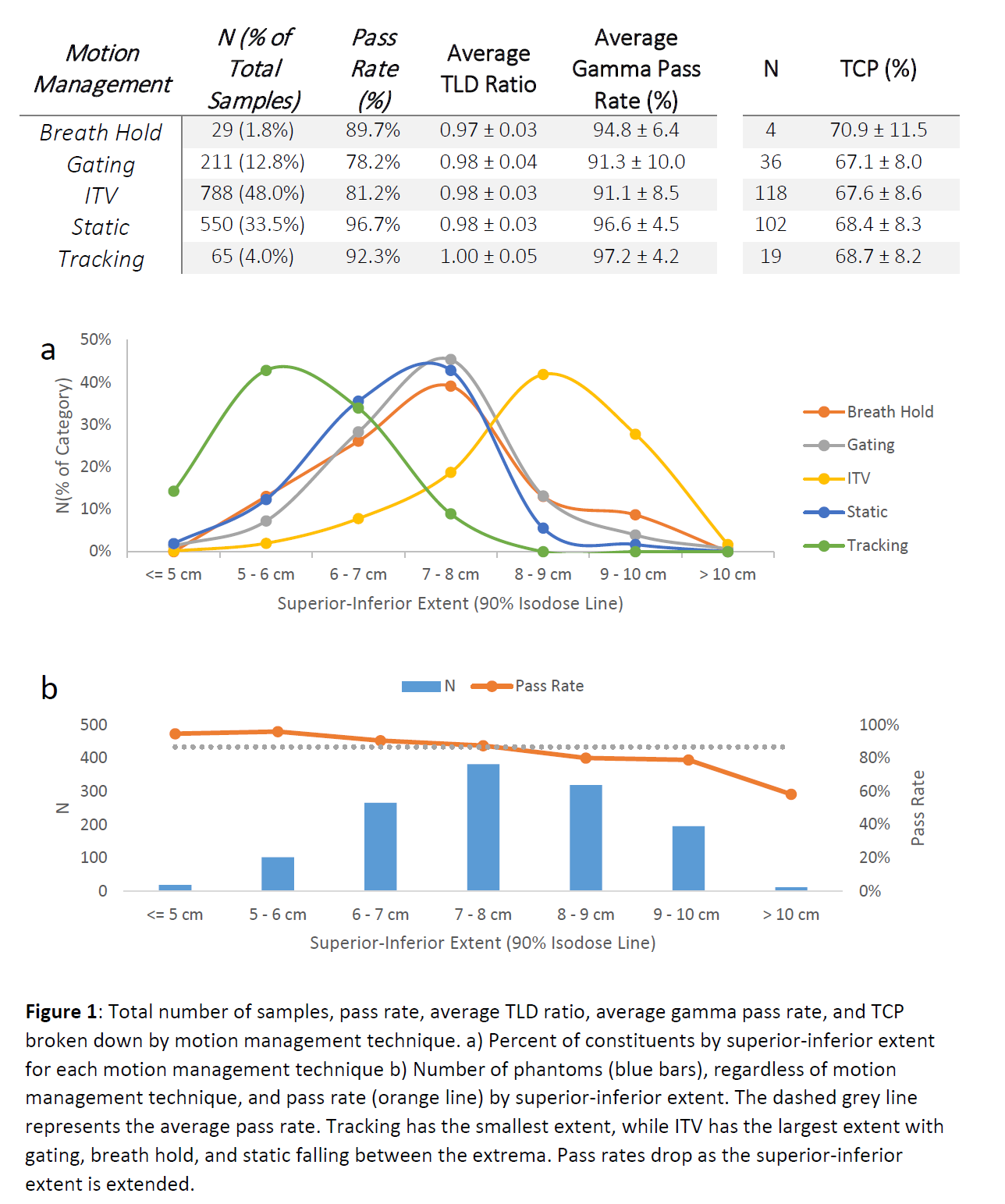
Conclusion
Motion management technique played an important role in the passing or failing result of IROC’s thoracic phantom. In a counter-intuitive finding, the use of larger radiation fields to cover the target was associated with poorer performance in delivering the treatment as intended. Clinically, careful attention to the choice of motion management technique and its implementation is needed to ensure optimal patient care.