On the configuration of small SRT beams: a protocol for accurate parameterization of a beam model
MO-0476
Abstract
On the configuration of small SRT beams: a protocol for accurate parameterization of a beam model
Authors: Mohammed Ghazal1,2, Tim Melhus3,4, Hamza Benmakhlouf1,2
1Karolinska University Hospital, Department of Medical Radiation Physics and Nuclear Medicine, Stockholm, Sweden; 2Karolinska Institute, Department of Oncology-Pathology, Stockholm, Sweden; 3Stockholm University, Medical Radiation Physics, Department of Physics, Stockholm, Sweden; 4Karolinska University Hospital, Department of Radiotherapy, Stockholm, Sweden
Show Affiliations
Hide Affiliations
Purpose or Objective
Most TPSs utilize parameterized multi-source models which are configured during commissioning, to represent the radiation beam of linacs. However, small-field stereotactic beams require special attention due to the importance of correct spot- and field-size definition. The purpose of this work is to develop a protocol for configuring a beam model that provides accurate representation of stereotactic beams.
Material and Methods
This work was based on 6 MV FFF beams as a proof of concept of the proposed protocol. Lateral beam profiles were measured in water using a small-field detector (IBA Razor diode) at various depths (5 cm, 10 cm and 20 cm) and for MLC-collimated field sizes: 2 x 2 cm2 - 5 x 5 cm2. These profiles served as a reference against which the beam model was optimized by configuring: (i) the Dosimetric Leaf Gap (DLG) and (ii) the Effective Spot Size (ESS). The optimization was performed by calculating the Absolute Integrated Difference (AID) between measured and modelled profiles in the penumbra region, finding the parameters which produce the lowest AID. This was evaluated by measuring 19 clinical SRT treatment arcs using the Electronic Portal Imaging Device and compare them with corresponding modelled arcs produced by both the standardly configured clinical model and the SRT-optimized model of this work. The proposed protocol was implemented on AAA and Acuros XB in the Eclipse TPS.
Results
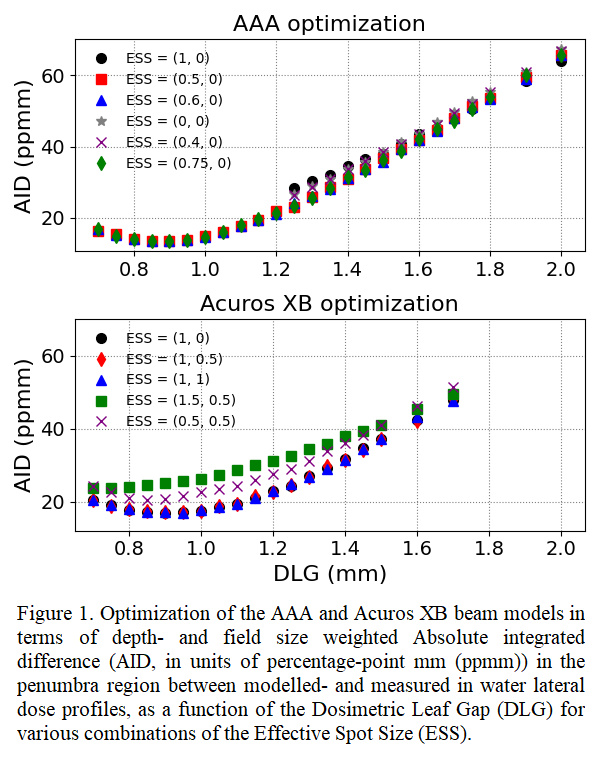
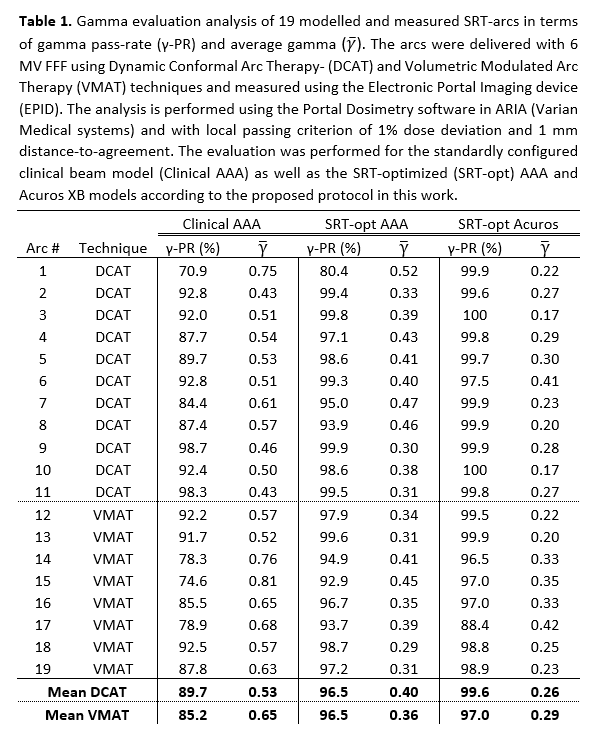
Figure 1 shows the field size- and depth-weighted AID between measured and modelled profiles against the DLG for various ESS. Significant improvement in the agreement between measured and modelled profiles are easily identified using the suggested protocol. DLG-variations greatly impact the AID as it is calculated in the penumbra region where the DLG is critical. ESS-variations are less impactful on the AID because their influence is field size-dependent. The DLG was determined at an optimum of 0.9 mm for both models whereas the ESS was determined to be (0.5, 0) mm and (1, 0,5) mm for AAA and Acuros XB, respectively. Comparison between measured and modelled SRT arcs was performed using gamma analysis with a local passing criterion of 1% and 1 mm. Table 1 presents the data of each arc comparison with corresponding gamma pass-rate and average gamma. Compared to the standardly configured clinical model, the SRT-optimized AAA (Acuros XB) model showed an average of 13% (14%) and 8% (11%) higher gamma pass-rates for VMAT- and DCAT arcs, respectively.
Conclusion
The insufficient modelling of treatment head components coupled with small-field physics phenomena necessitate the use of approximations in the Eclipse TPS which must be quantified and optimized meticulously for an accurate representation of the stereotactic beam. The current standard protocol for TPS commissioning was shown to produce a non-optimal beam model for small treatment volumes compared to the model given by the proposed protocol in this work which results in a significantly better representation of the stereotactic beam.