HPV subtypes and integration not prognostic in p16+ oropharyngeal squamous cell carcinoma
Jacob Lilja-Fischer,
Denmark
MO-0870
Abstract
HPV subtypes and integration not prognostic in p16+ oropharyngeal squamous cell carcinoma
Authors: Jacob Lilja-Fischer1, Morten Horsholt Kristensen1, Torben Steiniche2, Trine Tramm2, Jesper Grau Eriksen1, Jens Overgaard1, Magnus Stougaard2
1Aarhus University Hospital, Experimental Clinical Oncology, Aarhus, Denmark; 2Aarhus University Hospital, Department of Pathology, Aarhus, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Treatment response and prognosis after primary (chemo-)radiotherapy for oropharyngeal squamous cell carcinoma (OPSCC) is affected by Human Papillomavirus (HPV) status, with a markedly better prognosis in HPV-positive OPSCC. There are numerous HPV subtypes, and it is still debated if prognosis depends on this. Further, HPV DNA may be integrated into the host genome, or exist episomally. Some studies have indicated that prognosis may be worse if HPV DNA is fully integrated. These aspects are as of yet not fully settled, and are not in routine clinical use.
Purpose of this study was: 1) Validation of a custom-made targeted HPV next generation sequencing (NGS) panel in OPSCC; 2) determine correlation with p16 immunohistochemistry (IHC) 3); characterize HPV types and integration status; 4) assess impact on outcome in a contemporary cohort treated in a rigorous protocol.
Material and Methods
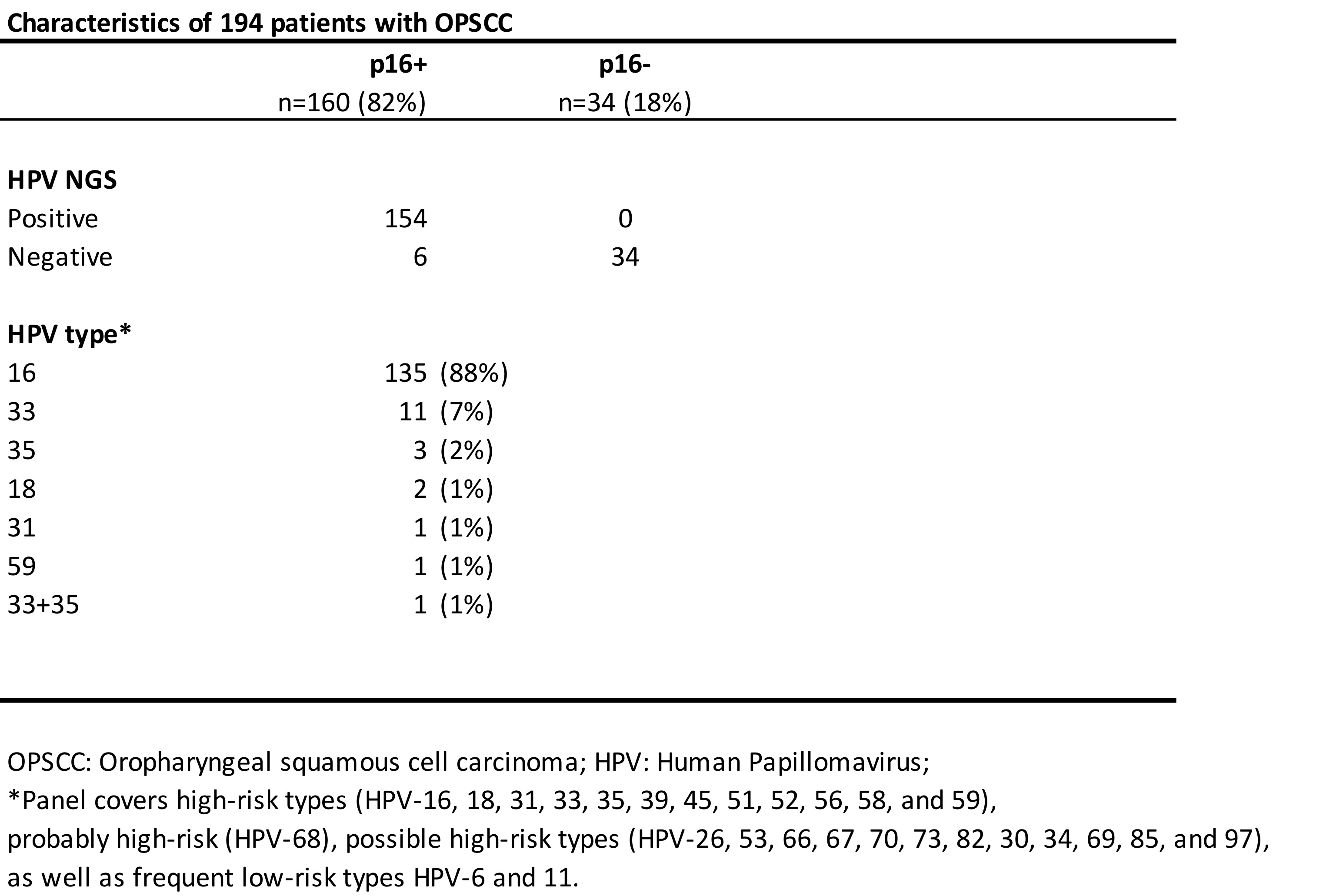
We included a total of 194 patients with OPSCC treated with primary (chemo-)radiotherapy according to DAHANCA guidelines. Of these, 160 (82%) were p16-positive, and 34 (18%) p16-negative.
HPV-status was determined by targeted HPV next generation sequencing (NGS), using a custom-made genotyping panel covering all 25 carcinogenic, probably carcinogenic, and possibly carcinogenic HPV types. Furthermore, the NGS panel was designed to detect HPV integration status.
Results
HPV was detected in 154 tumor samples. p16 IHC and NGS HPV status were concordant in 188 (97%) of 194 patients, whereas we did not detect HPV DNA in 6 p16+ tumors (See table).
HPV16 accounted for 135 of 154 HPV-positive cases (88%). HPV33 was found in 11 patients (7%). HPV types 18, 31, 35 and 59 were also detected.
We found evidence of complete integration of HPV sequence into the host genome in 14 patients (7%). Integration status did not depend significantly on HPV type.
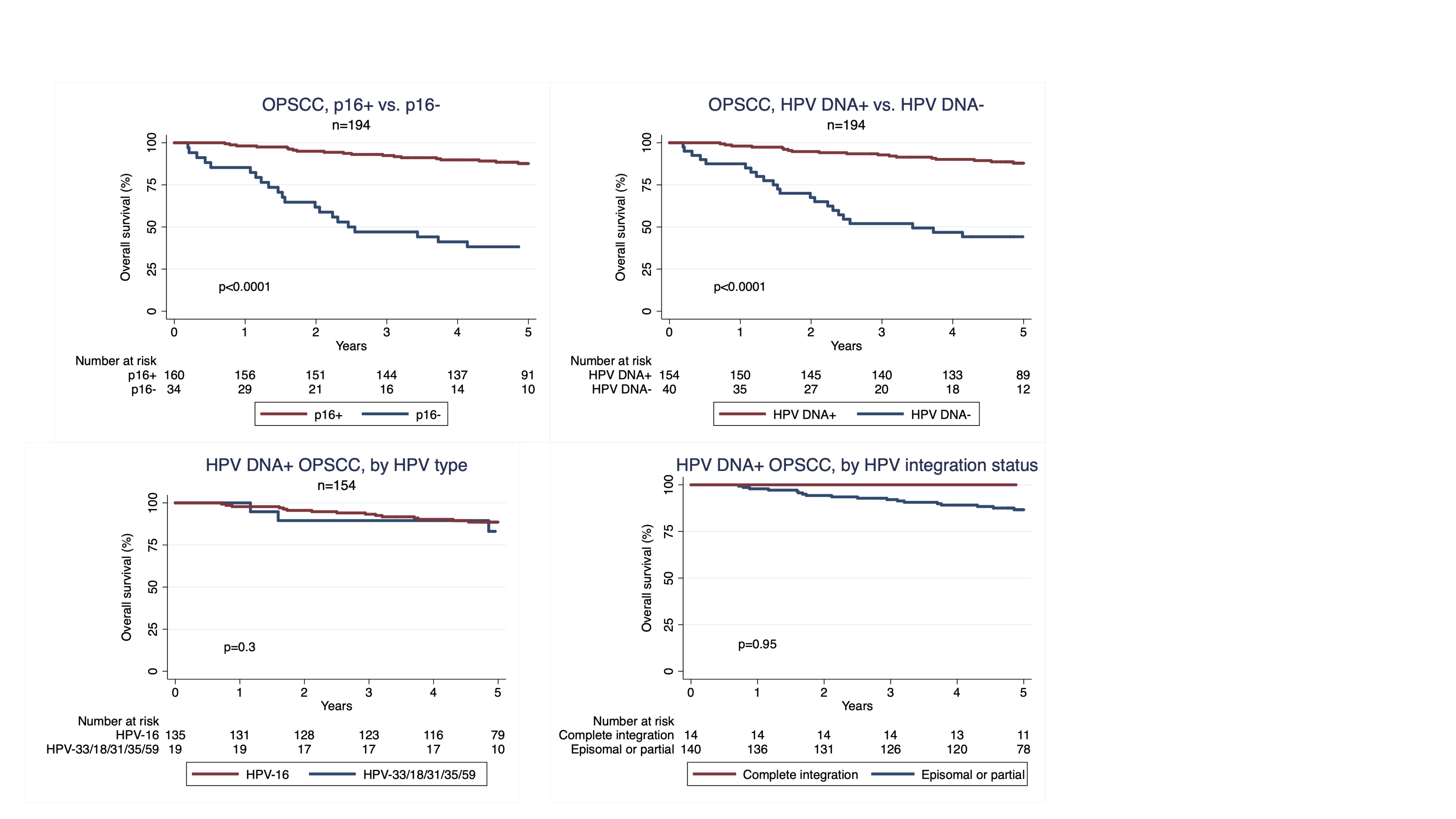
Overall survival was similar whether patients were separated by p16 IHC, or HPV DNA status (p<0.0001 for both). Overall survival did not depend on HPV type, or HPV DNA integration status (p=0.3 and p=0.95, respectively).
Conclusion
We successfully validated use of a targeted HPV NGS panel in HNSCC, with very high concordance with p16 IHC, and ability to detect HPV integration status. HPV type and integration status hold no prognostic information after primary (chemo-)radiotherapy, in a contemporary cohort treated to a uniformly high standard.
p16 IHC still remains a valid and sufficient prognostic biomarker in OPSCC.