The virtual reality for managing emotional distress in paediatric patients receiving radiotherapy
MO-0557
Abstract
The virtual reality for managing emotional distress in paediatric patients receiving radiotherapy
Authors: Soraya Mico1, David Garcia2, Monica Ramos3, Anna Salo4, Marina Boufill5, Eugenia Bustelo5, Josep Garre3, Enar Recalde3, Jordi Giralt3
1Hospital Universitario Vall D´Hebron , Radiation oncology , Barcelona , Spain; 2Hospital Universitario Vall D´Hebron, Radiotherapy oncology technician , Barcelona, Spain; 3Hospital Universitario Vall D´Hebron, Radiation oncology, Barcelona, Spain; 4Hospital Universitario Vall D´Hebron, Psychologist , Barcelona, Spain; 5Hospital Universitario Vall D´Hebron, Psychologist, Barcelona, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiotherapy treatment in paediatric patients could cause emotional distress such as fear, anxiety and refusal, so some of the youngest patients have to be treated under anaesthesia. A previous understanding of the procedure with the immersive virtual reality (IVR) can help to prevent these symptoms.
Material and Methods
Paediatric patients treated with radiotherapy during April 2021 to October 2021 received an IVR Kit that included a cardboard headset, and web-app access to a 360-degree video of the radiotherapy facility and the treatment procedure. The 360º IVR experience was created combining 360º images of real hospital environments (including real human figures) and “Nixi”, a 3D animated character that acted as the patient (Nixi for children, Barcelona). The IVR experiences were designed by the Nixi for Children team together with professionals and patients within the framework of the "I'm Ready project", created in collaboration with The Ricky Rubio Foundation. This video was given after the first medical appointment and patients could watch it as many times as they needed from that moment until the first day of radiotherapy. A psychological survey of the emotional status in relation to the treatment was conducted after the first medical appointment, after the CT-simulation and after the first day of treatment. The psychological surveys were oriented to collect the patient's own assessment, the vision of the relatives and the radiotherapy technicians.
Results
22 patients received the IVR. Only 9 completed the surveys correctly. The clinical characteristics are described in Table 1. Only one patient was older than 12 years and 4 of them were between 3-5 years old. 56% of the relatives who answered the survey detected discomfort in the children that could be relieved with the help of an adult previous to the first consultation, 30% previous to the CT-simulation and only 11% previous to the beginning of radiotherapy. Of the symptoms surveyed, patients most frequently show fear, anxiety and nervousness, which progressively decrease until the day of the first treatment (4 patients were afraid previous to the first visit, 3 previous to the CT-simulation and none previous to the treatment/ 3 patients had anxiety prior to the first visit, 1 prior to CT-simulation and none prior to treatment/ 4 patients had nervousness prior to the first visit, 3 prior to CT-simulation and 2 prior to treatment). According to the children's evaluation, 75% were calm before the first consultation and showed an improvement of up to 87.5% prior to the simulation. Two patients required anaesthesia on the day of the CT-simulation, but all of them were finally treated without anaesthesia.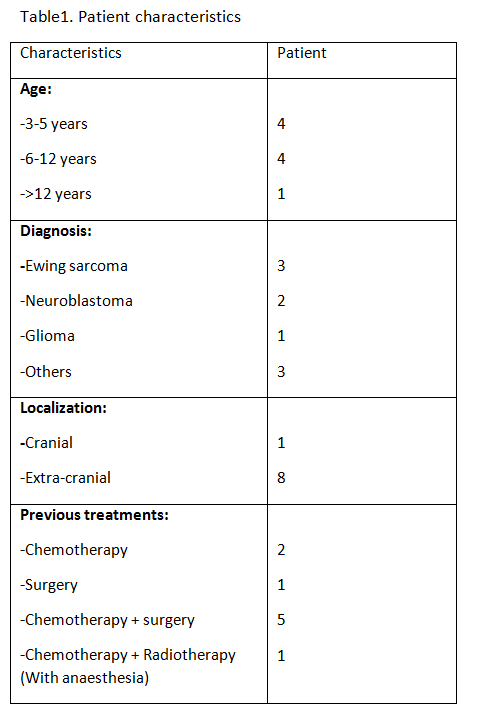
Conclusion
A 360-degree video tour using a virtual reality system helps to reduce children's discomfort before radiotherapy treatment. The reduction of fear, anxiety and nervousness in children can contribute to decrease the need of sedation for treatment.