Time trends for online adapative treatment on the 1.5T MR-Linac
Jasmijn Westerhoff,
The Netherlands
MO-0148
Abstract
Time trends for online adapative treatment on the 1.5T MR-Linac
Authors: Jasmijn Westerhoff1, Lois A. Daamen1, Eline N. de Groot-van Breugel2, Jochem R. N. van der Voort van Zyp2, Joost J. C. Verhoeff2, Stella Mook2, Helena M. Verkooijen1, Martijn P. W. Intven2
1University Medical Centre Utrecht, Division of Imaging and Oncology, Utrecht, The Netherlands; 2University Medical Centre Utrecht, Department of Radiation Oncology, Utrecht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
One of the major advantages of a hybrid linear accelerator with MRI (MR-Linac) is the ability to use an online adaptive workflow. With this workflow (i.e. Adapt-To-Shape (ATS) for the 1.5 Tesla (T) MR-Linac) treatment accuracy is increased by manually adjusting delineations of target and organs at risk just before dose delivery. However, manually adjusting delineations increases treatment time. First studies show that it is feasible to treat most fractions using ATS in less than 60 minutes, but these studies mainly report on the first treatments of each institute. The aim of this study is to assess the time trends in duration of treatment fraction using the ATS workflow on an MR-Linac for treatment of prostate cancer, rectal cancer, and lymph nodes metastases by looking at the duration of the preparation phase (DPP) of the fraction. In addition, we describe the influence of switching to an RTT-led workflow DPP.
Material and Methods
This monocenter study was conducted using the Multi-OutcoMe EvaluatioN of radiation Therapy Using the MR-Linac (MOMENTUM) cohort (NCT04075305). Included were all patients who received treatment on the Unity 1.5T MR-Linac (Elekta, Stockholm) for prostate cancer, rectal cancer, or LNM using the ATS workflow. Patients that participated in an interventional trial were excluded. The ATS workflow was primarily led by RO, however, delineation adjustments were led by trained RTT’s since December 2019 for LNM, and since January 2020 for prostate and rectal cancer. DPP was defined as the interval between start of pretreatment scan and start of position verification scan, obtained from DICOM data of the acquired MRI’s. This represents the duration of the first MRI scan, registration of images, matching of contours, and manual adaptation of the delineation. Duration of the first MRI scan was a constant factor over time, but the duration of image registration and delineation were variable. The mean change in DPP per year was calculated using one-way analysis of variance (ANOVA). A p-value < 0.05 was considered statistically significant.
Results
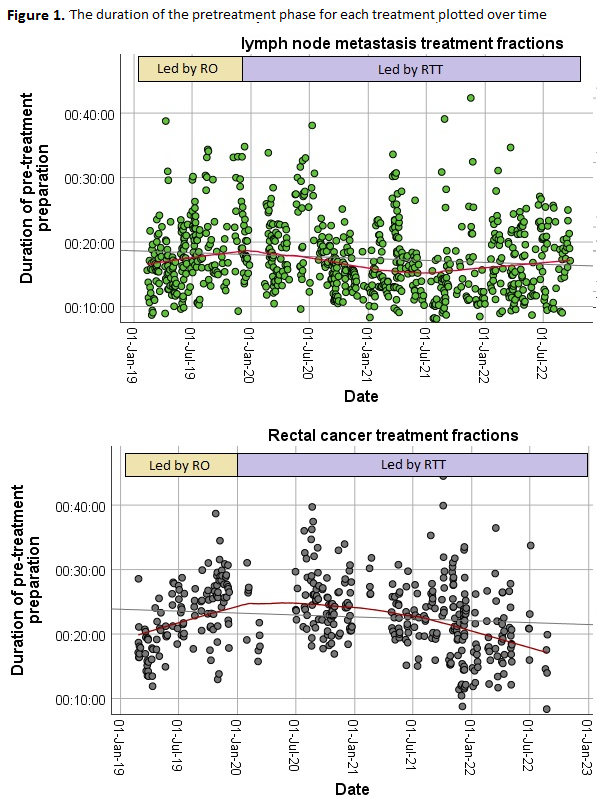
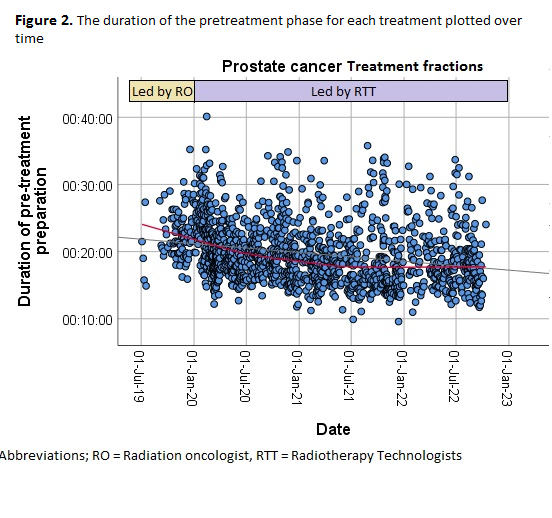
The analysis included 1541 treatment fractions (310 patients) for prostate cancer, 408 treatment fractions (82 patients) for rectal cancer, and 778 treatment fractions (153 patients) for LNM. Mean DPP was 19:45 min (standard deviation (SD) 04:30) for prostate cancer, 23:04 min (SD 05:20) for rectal cancer and 17:33 min (SD 05:35) for LNM. The DPP for each treatment was plotted over time (Figure 1 and 2). A significant change in mean DPP per year was found for prostate cancer (p < 0.001), rectal cancer (p < 0.001) and LNM (p=0.001).
Conclusion
This study shows that DPP for the application of ATS workflows decreases over time for prostate and rectal cancer treatment and remains stable for treatment of LNM. The introduction of an RTT-led workflow did not increase DPP.