Impact of the 2022 UK Consensus dose-volume constraints on national SBRT benchmark planning
Mariana Kroiss,
United Kingdom
MO-0145
Abstract
Impact of the 2022 UK Consensus dose-volume constraints on national SBRT benchmark planning
Authors: Mariana Kroiss1, Patricia Díez1, Rushil Patel1
1National Radiotherapy Trials Quality Assurance Group, Mount Vernon Cancer Centre , Radiotherapy Physics, Northwood, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Use of SBRT techniques for the treatment of oligometastases has been rolled out nationally since July 2020, and a radiotherapy QA program was put in place to ensure safe and consistent implementation. Planning benchmark cases for 6 anatomical sites (bilateral lung, liver, adrenal, iliac bone, bilateral pelvic node and lumbar spine) were circulated for SBRT accreditation as part of the QA program. An updated, more conservative, UK Consensus on normal tissue dose-volume constraints for SBRT (Diez et al, 2022) was recently published and its impact on plan acceptability for oligometastatic disease is evaluated.
Material and Methods
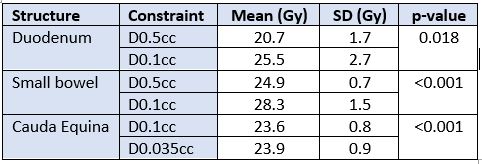
The 6 benchmark cases were inspected and those with structures overlapping the PTV evaluated for compliance with updated constraints. Specifically, duodenum was assessed for the liver case, small bowel for the nodal case and cauda equina for the spinal case. A total of 59 approved SBRT benchmark plans (7 liver, 31 node and 21 spine) were reviewed. Dose prescriptions for these cases were 45 Gy, 30 Gy and 27 Gy for liver, node and spine, respectively, all in 3 fractions. All OAR dose-volume constraints satisfied existing guidance (Hanna et al, 2018). Dose to the duodenum (D0.5cc <22.2 Gy), dose to small bowel (D0.5cc <25.2 Gy) and dose to cauda equina (D0.1cc <24.0 Gy) were reviewed. Changes introduced by the 2022 Consensus for these structures were in terms of near-maximum volumes. These were reduced from 0.5 cc and 0.1 cc to 0.1 cc and 0.035 cc for luminal structures and cauda equina, respectively. A Wilcoxon sign rank test was performed to evaluate differences between the 2 sets of constraints.
Results
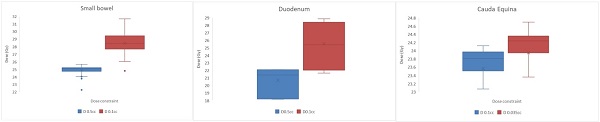
5/7 liver plans and 30/31 nodal plans failed to achieve the D0.1cc constraint for duodenum and small bowel, respectively. 13/21 spine plans did not achieve the D0.035cc constraint for cauda equina. Mean near-maximum doses for each structure, for each set of constraints is detailed in Table 1. Differences observed between the 2018 and 2022 dose-volume constraints were found to be statistically significant.
Table 1: Mean near-maximum doses achieved for the 2018 and 2022 Consensus constraints
Conclusion
The effect of applying updated dose-volume constraints to normal tissues from existing benchmark submissions was assessed. The new constraints should not significantly impact planning unless OARs are adjacent or overlapping the PTV. 71 % of liver plans, 97% of nodal plans and 62 % of spine plans would have required re-optimisation. An already very steep dose gradient between target and cauda equina in most spine plans is reflected in the lower failure rate. Steeper gradients may be necessary in planning other anatomical sites where OARs are adjacent to the target.
Figure 1: Variation in near-maximum doses as defined in the 2018 (D0.5cc) and 2022 (D0.1cc) Consensus guidelines