Nationwide RT trends & variation in locoregional M0 breast cancer treatment in NL – 2008 until 2019
Jelle Evers,
The Netherlands
MO-0138
Abstract
Nationwide RT trends & variation in locoregional M0 breast cancer treatment in NL – 2008 until 2019
Authors: Jelle Evers1,2, Maurice Van der Sangen3, Marissa Van Maaren2,1, Monique Bloemers4, Desiree Van den Bongard5, Luc Strobbe6, John Maduro7, Mieke Aarts1, Henk Struikmans8, Sabine Siesling1,2
1Netherlands Comprehensive Cancer Organisation, Department of Research and Development, Utrecht, The Netherlands; 2University of Twente, Department of Health Technology and Services Research, Enschede, The Netherlands; 3Catharina Hospital, Department of Radiation Oncology, Eindhoven, The Netherlands; 4The Netherlands Cancer Institute, Department of Radiation Oncology, Amsterdam, The Netherlands; 5Amsterdam University Medical Center, Department of Radiation Oncology, Amsterdam, The Netherlands; 6Canisius Wilhelmina Hospital, Department of Surgical Oncology, Nijmegen, The Netherlands; 7University Medical Center Groningen, Department of Radiation Oncology, Groningen, The Netherlands; 8Leiden University Medical Center, Department of Radiation Oncology, Leiden, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Describing nationwide trends and variation in radiotherapy (RT) use in the context of locoregional non-metastatic (M0) breast cancer treatment in the Netherlands from 2008 until 2019.
Material and Methods
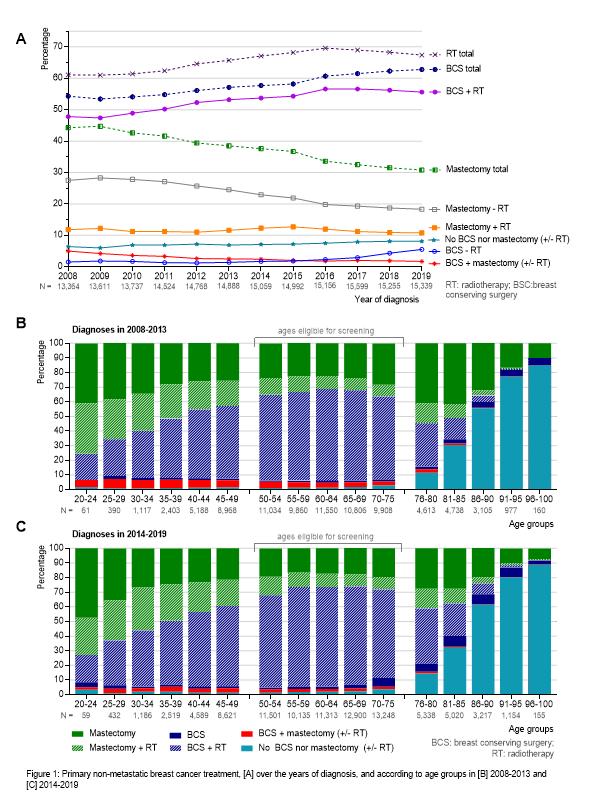
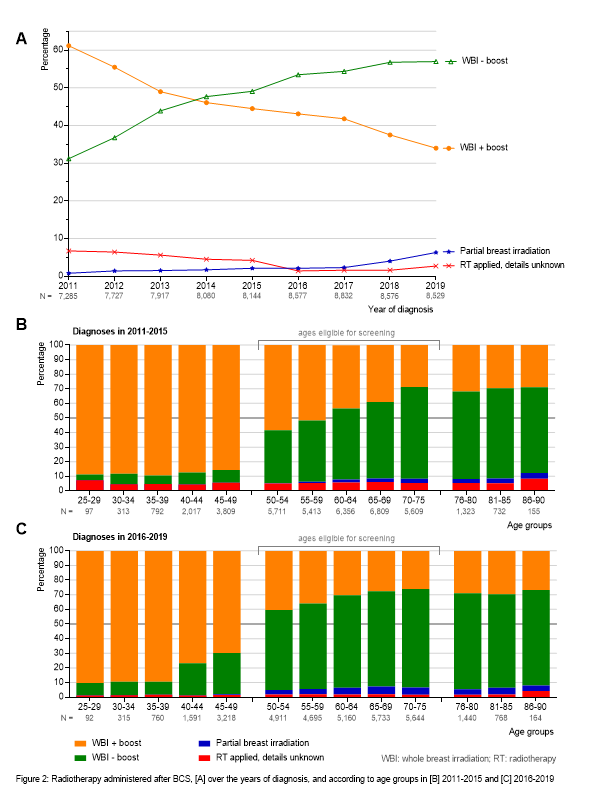
Women diagnosed with M0 breast cancer in 2008-2019 were selected from the population-based Netherlands Cancer Registry. Primary treatment was presented over time. Non-specified RT use was available in all study years. RT details were available from 2011. Use of whole breast irradiation (WBI) with boost/WBI without boost/partial breast irradiation (PBI) were presented in women who underwent breast conserving surgery (BCS). Multilevel logistic regression analyses were applied to identify variables associated with (1) post-BCS WBI with boost versus without, and (2) regional RT versus axillary lymph node dissection (ALND) in women with N+ disease.
Results
During 2008-2019, 176,292 women were diagnosed with M0 breast cancer in the Netherlands. An increasing percentage received RT in 2008 (61%)–2016 (70%), caused by a shift from mastectomy to breast conserving therapy and increased post-mastectomy RT use (Fig 1A). After 2016, RT use slightly decreased to 67%, as women aged ≥70yrs more frequently received BCS without RT (Fig 1B/C). RT de-escalation was also observed by increased PBI use and decreased boost RT use following WBI (Fig 2). Older women (>75vs<50yrs OR:0.04, 95%CI:0.03-0.05) were less likely to receive boost RT, while women with N+ or higher grade disease (pN+ vs pN0 OR:1.46 95%CI:1.32-1.60 / grade III vs I OR:11.46, 95%CI:9.90-13.26) or residual tumour (focal R1 vs R0 resection OR:28.08, 95%CI:23.07-34.17) had an increased probability of receiving boost RT. Variation in boost RT was observed between regions of residence but could not be explained by hospital characteristics. In women with N+ disease, increased regional RT use (32% in 2011-61% in 2019) coincided decreased ALND use (76% in 2011-24% in 2019). Women aged >75yrs least often received regional treatment and were less likely to receive regional RT instead of ALND (>75vs<50yrs OR:0.68, 95%CI:0.95-0.78). Also, women with poorer WHO performance status, higher T-stage or grade, or >30 minutes travel time for RT less likely received regional RT instead of ALND, while women with lymph node micrometastases more likely received regional RT. N+ treatment varied between regions of residence (Southwest vs North OR:0.55, 95%CI:0.37-0.80) but not for hospital characteristics.
Conclusion
RT use in primary M0 breast cancer treatment increased until 2016 and slightly decreased afterwards. Clinical practice has de-escalated treatment as RT following BCS was more often omitted in older women, PBI use increased, and boost RT following post-BCS WBI strongly decreased. Boost RT varied for patient and disease characteristics and by region. N+ disease became frequently treated with regional RT instead of ALND, which use varied for women’s age, performance, disease characteristics, RT travel time and region of residence.