Dose to heart substructures is associated with grade≥3 cardiac events after SABR in stage I–II NSCLC
MO-0643
Abstract
Dose to heart substructures is associated with grade≥3 cardiac events after SABR in stage I–II NSCLC
Authors: Marzia Cerrato1, Fabio Menegatti1, Ilaria Bonavero1, Chiara Casale1, Cristiano Grossi1, Serena Badellino1, Ramona Parise1, Umberto Ricardi1, Mario Levis1
1University of Turin, Department of Oncology, Turin, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
The aim of this prospective study is to investigate for any existing association between the dose delivered to heart substructures and OS, non-tumor-related survival, and the development of cardiac toxicity, in early stage (ES) NSCLC patients treated with SABR.
Material and Methods
Patients with PS ECOG score 0-1 and no previous radiation treatment to the mediastinum were included. Details on pre-existing cardiovascular risk factors and comorbidities, ongoing pharmacological therapies and lung function tests were collected at baseline. Cardiac substructures (chambers, and coronary arteries) were prospectively contoured in order to collect dosimetric data. Cardiac events (CEs) were evaluated with the CTCAE 5.0 grading. Cox regression model was used to assess associations between covariates and CEs. The Fine and Gray competing risk regression model was used to predict the cumulative incidence of grade (G) ≥ 3 CEs considering non-cardiac death as a competing risk.
Results
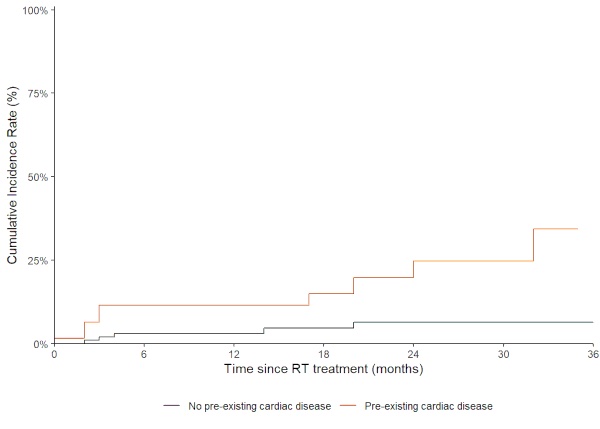
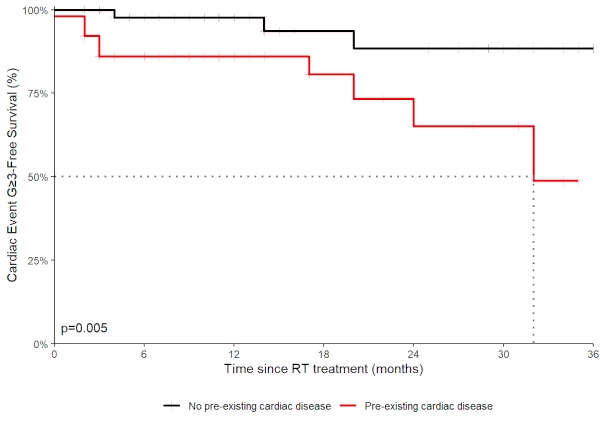
From March 2019 to September 2022, 104 patients were enrolled with a median age of 76 years. The median overall survival (OS) was of 34 months (1-year OS: 83%; 2 year-OS 65%). Death was documented in 28 (27%) patients, in 14 (50%) for non-neoplastic causes. 51 (49%) patients had a pre-existing cardiac disease. Overall, 21 patients (20%) developed at least one CE during the follow-up and 15 patients had a first CE of G ≥ 3 at a median of 4 months (Interquartile Range: 2.5 to 20 months). Cox multivariable analysis shows that pre-existing cardiac disease (hazard ratio [HR]: 5.86; p= 0.008), mean right atrium (RA) dose (HR: 1.28, p= 0.01) and descendent aorta dose (10 cc) (HR: 1.08, p= 0.017) were associated with the development of a G ≥ 3 CE. Patients with pre-existing heart conditions had a higher cumulative incidence of the first G ≥ 3 CE (12 months- cumulative incidence was 11% and 3.1 %, respectively; p=0.001) (Figure 1) and a decreased G≥ 3 Cardiac Event-Free Survival (p=0.005) (Figure 2) compared to patients without any cardiac comorbidity. In competing-risk multivariable analysis, pre-existing cardiac diseases (HR: 4.32; p= 0.046), mean RA dose (HR:1.22; p=0.007) and diuretic therapy (HR: 2.57, p= 0.040) showed a statistically significant association with G ≥ 3 CEs. However, the development of a G ≥ 3 CE did not affect OS (p=0.4). Heart doses were not associated with non-tumor-related survival or OS.
Conclusion
In this interim analysis of the first ever prospective study investigating cardiac toxicity of SABR in ES-NSCLC patients, we observed that pre-existing cardiac diseases, mean RA dose and diuretic therapy increase the risk of developing G ≥ 3 CEs. Our actual results suggest a possible correlation between heart dosimetry and the development of SABR related cardiac toxicity. Completion of the patient accrual and longer follow up are required to confirm these results and to investigate for a potential impact on OS.