Predicting post-radiotherapy cardiac toxicity for non-small cell lung cancer patients
Zhuoyan Shen,
United Kingdom
MO-0642
Abstract
Predicting post-radiotherapy cardiac toxicity for non-small cell lung cancer patients
Authors: Zhuoyan Shen1, Maria A. Hawkins1,2, Douglas Brand1,2, Ying Zhang1, Olivia Chohan2,1, John Watts1, Mikael Simard1, Charles-Antoine Collins Fekete1
1University College London, Department of Medical Physics and Biomedical Engineering, London, United Kingdom; 2University College London Hospitals NHS Foundation Trust, Department of Radiotherapy, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Cardiac toxicity after thoracic radiotherapy (RT) for lung cancer is a potentially lethal side effect. Long term outcomes from the RTOG-0617 dose-escalation trial show that higher dose to the heart is associated with shorter overall survival. However, models incorporating risk factors beyond dosimetry may better predict cardiac events. Here we apply artificial intelligence (AI) methods incorporating clinical, anatomical and dose data to model cardiac events in RTOG-0617.
Material and Methods
(1) Data: The RTOG-0617 trial compared standard dose (60 Gy) vs high dose (74 Gy) radiotherapy for stage III non-small cell lung cancer (NSCLC) patients receiving chemo-RT (concurrent Paclitaxel ± Cetuximab). The data of 404 trial participants was used for model training (70%), validation (15%) and hold-out testing (15%). Patients with grade 3+ adverse events (graded by CTCAE version 3.0) related to heart were labelled as positive (37/404, 9.2%).
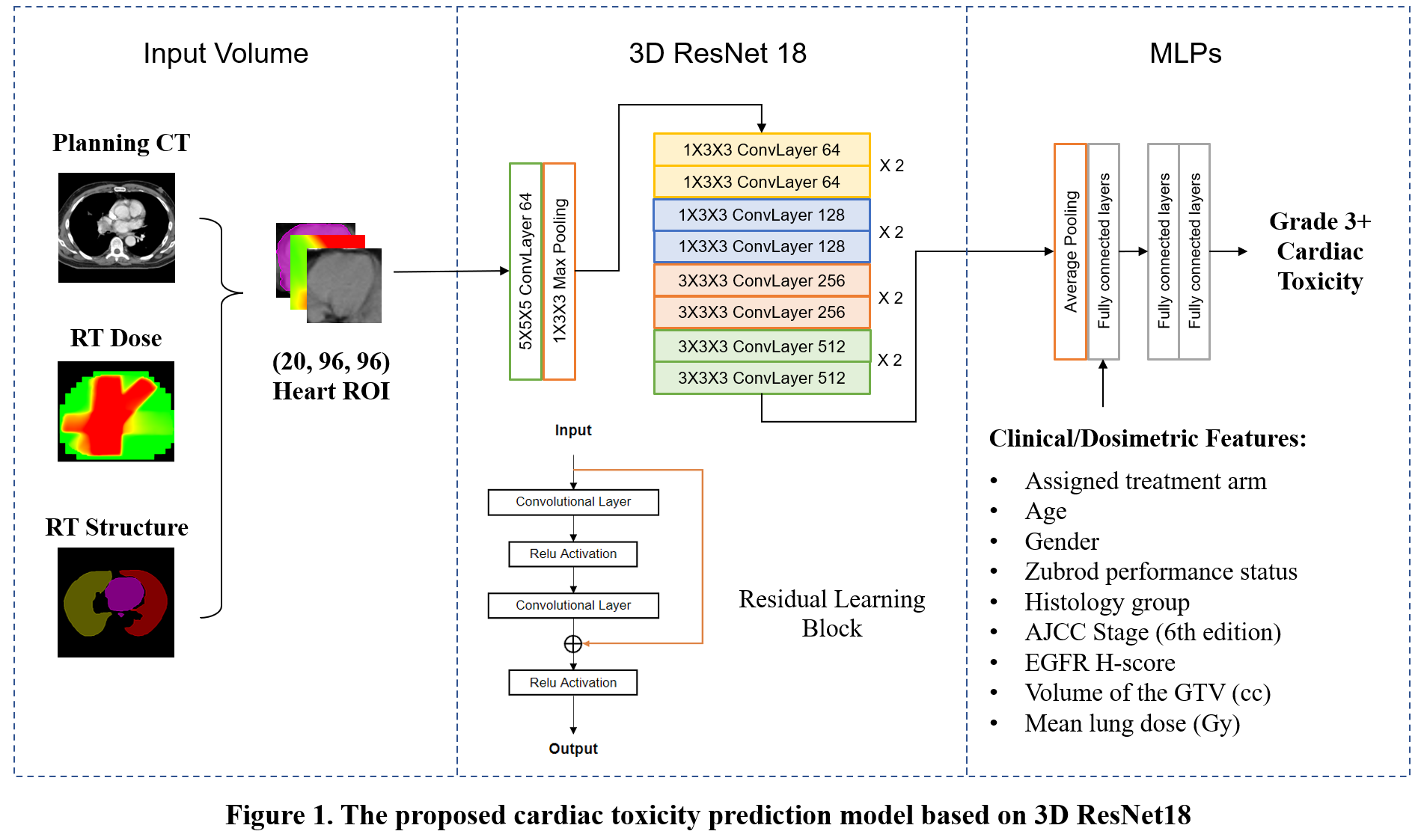
(2) Methods: The planning CT scan, RT dose map and heart contour of the patients were combined as three-channel 3D volumes with a shape of (20 slices, 96 pixels, 96 pixels). A pretrained 3D ResNet18 processed the three-channel image input, and nine selected features were integrated by fully connected layers. The concatenated output was processed by multilayer perceptrons (MLPs) to predict the binary toxicity label. The architecture of the whole model is illustrated in Figure 1.
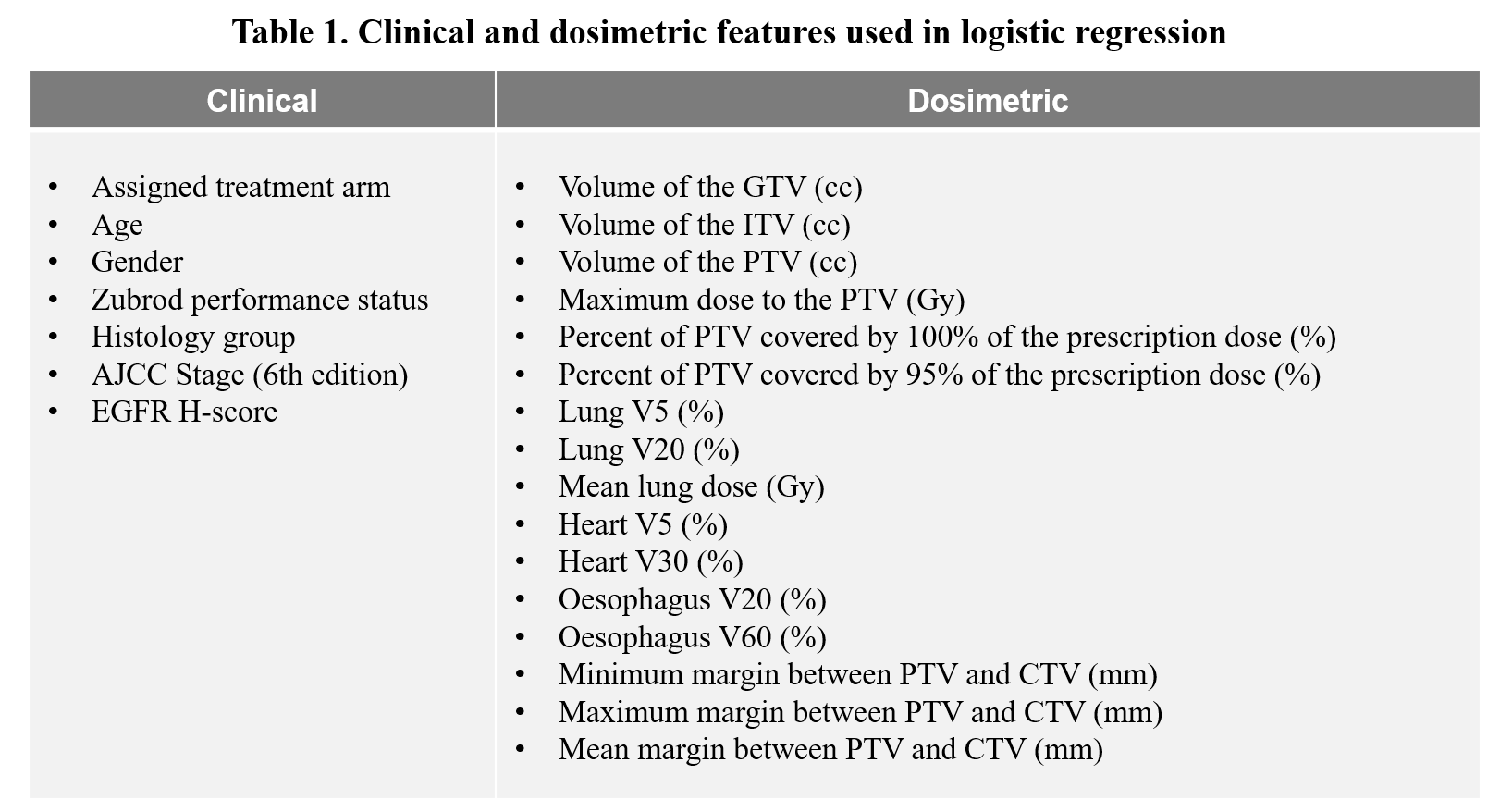
The AI model was compared to a multivariate logistic regression model trained with clinical variables and dosimetric parameters listed in Table 1.
Results
Our AI model yielded an area under the receiver operating characteristic curve (AUC) of 0.714 (95% CI: 0.693 – 0.734) on the hold-out dataset after bootstrapping with 50 iterations. The AUC for the standard dose and high dose subsets were 0.696 (95% CI: 0.685 – 0.721) and 0.721 (95% CI: 0.705 – 0.738), respectively. The AUC for our model was significantly higher (p < 0.001) than the logistic regression model trained using only clinical and dosimetric variables (AUC: 0.597 ; 95% CI: 0.582 – 0.621). The overall AUC of our model went up to 0.747 (95% CI: 0.726 – 0.768) by ensemble voting using the top five bootstrap models (ranked by AUC) .
Conclusion
We developed an AI model to predict post-treatment cardiac toxicity for NSCLC patients receiving chemo-RT. The model significantly outperformed conventional logistic regression analysis. The predictive accuracy may be improved by expanding the training dataset and developing a model specific to patients treated with standard RT doses. Future work aims to: (1) Expand the model to predict oesophageal and pulmonary toxicities; (2) Externally validate predictions on a real-world dataset, initially on a cohort being collected at University College London Hospitals.