Salvage HDR interventional radiotherapy for prostate cancer after prostatectomy and irradiation
MO-0300
Abstract
Salvage HDR interventional radiotherapy for prostate cancer after prostatectomy and irradiation
Authors: Tamer Soror1, Corrina Melcherta1, Dirk Rades1, Axel S Merseburger2, György Kovács3
1University of Lübeck, Radiation Oncology, Lübeck, Germany; 2University of Lübeck, Urology, Lübeck, Germany; 3Università Cattolica del Sacro Cuore, Gemelli-INTERACTS, Rome, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
to report on the technical feasibility, safety, and efficacy of interventional radiotherapy (IRT) with interstitial high-dose-rate (HDR) brachytherapy in the salvage irradiation for local recurrence after radical prostatectomy and subsequent external irradiation. To our knowledge, this is the first report on HDR-IRT in such a treatment setting.
Material and Methods
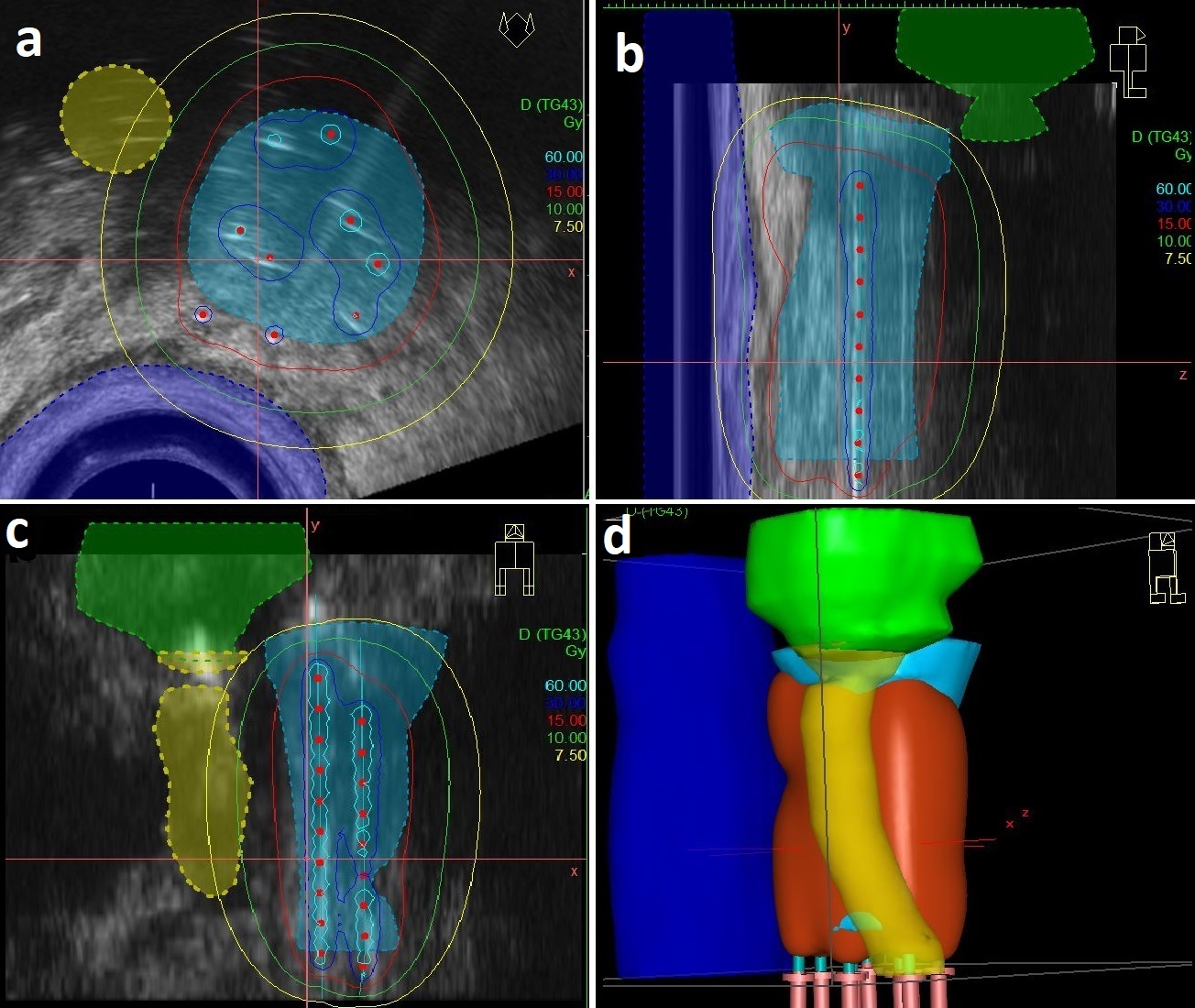
a retrospective study of patients with prostate adenocarcinoma treated with HDR-IRT for an isolated local relapse after prostatectomy and external irradiation at our institution (2010-2020). IRT was performed under general anesthesia with transrectal ultrasound guidance through a fixation template with a possible needle spacing of 3.3mm. Before HDR-IRT, a compatibility check is performed to exclude contraindications for HDR-IRT. Each patient received 30Gy in two fractions of HDR-IRT separated by 2 weeks. Biochemical failure following HDR-IRT is defined as a rise of 2 ng/mL or more above the PSA-nadir. PSA-nadir is the lowest reported level of PSA within 6 months after HDR-IRT. Treatment-related toxicities were graded according to the common terminology criteria for adverse events (CTCAE) 5.0.
Results
Ten patients were identified. The median age was 63 years (range: 59 – 74), with a median PSA value of 2.5 ng/mL (range: 0.4 – 2.7). All patients had received EBRT; six patients had the EBRT as an adjuvant treatment following surgery. Four patients had the EBRT as a salvage treatment for the local recurrence. In those four patients, the HDR-IRT was the second local salvage treatment after a further local progression. The median interval between EBRT and HDR-IRT was 42 months (range: 15 – 117).
The mean volume of the clinical target volume (CTV) as defined on TRUS images was 21.2cc (±7.9). The median number of needles inserted during the procedure was 8 (range:7 – 12). The mean CTV D90 was 93.7% (±2.4).
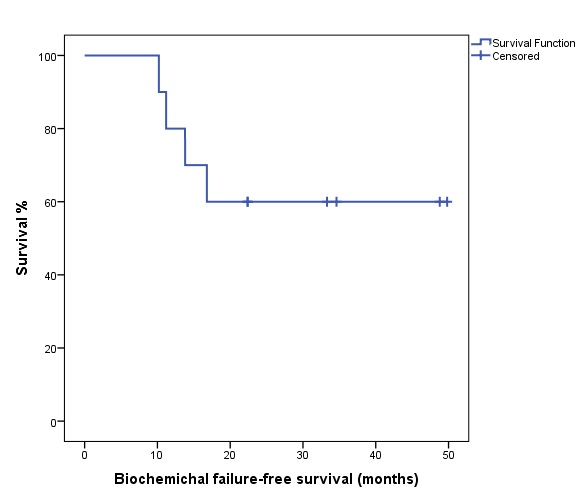
The median follow-up time is 34 months (range: 10 – 68). The PSA-nadir value following HDR-IRT was reached within six months with a median value of 0.2 ng/mL (range: 0.04 – 1.2). Biochemical failure following HDR-IRT was encountered in four patients; 3 patients showed a further progression of the local relapse, and one patient had evidence of distant metastases. The mean time to PSA-increase in these four patients was 13 months following HDR-IRT. The median biochemical failure-free survival (bFFS) for all patients was not reached. One-year (1-y) bFFS, 3-y bFFF, 4-y bPFF were 80%, 60%, and 60%, respectively. Most of the treatment-related toxicities were grade 1-2. Two patients had grade 3 late genitourinary toxicity.
Conclusion
HDR-IRT seems to be an effective treatment option with acceptable toxicity for prostate cancer patients with isolated macroscopic histologically confirmed local relapse after prostatectomy and subsequent external irradiation. Further clinical studies are encouraged to investigate the role of HDR-IRT in the management of local tumor relapse after RP.