Malnutrition is associated with poor survival in cervical cancer patients treated with radiotherapy
Janna Laan,
The Netherlands
MO-0047
Abstract
Malnutrition is associated with poor survival in cervical cancer patients treated with radiotherapy
Authors: Janna Laan1, Luc van Lonkhuijzen2, Karel Hinnen1, Bradley Pieters1, Inge Dekker3, Lukas Stalpers1, Henrike Westerveld1,4
1AmsterdamUMC, Radiation Oncology, Amsterdam, The Netherlands; 2AmsterdamUMC, Gynaecology, Amsterdam, The Netherlands; 3AmsterdamUMC, Nutrition and Dietetics, Amsterdam, The Netherlands; 4ErasmusMC, Radiation Oncology, Rotterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Patients treated with (chemo)radiotherapy with curative intent for cervical cancer are at risk for developing malnutrition, which consequently could have a negative effect on their prognosis. Nevertheless, only a few small studies have been published on this subject, all describing a non-Western European population not representative for our patients. Therefore, the aim of this study was to assess the incidence of malnutrition before, during and after external beam radiotherapy (EBRT) in cervical cancer patients treated in our centre. In addition, we evaluated the impact of malnutrition on survival and if and when malnourished patients were referred to a dietician.
Material and Methods
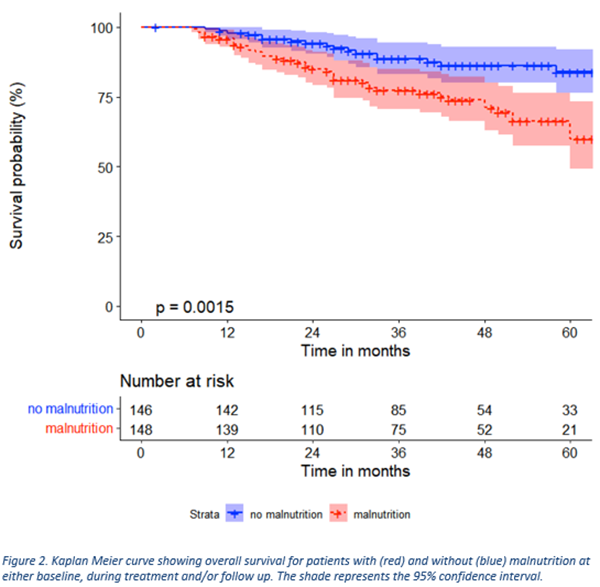
This retrospective cohort study included patients who received primary or adjuvant EBRT with curative intent for cervical cancer between 2013 and 2021. Patient and treatment characteristics, including longitudinal data on weight and dietary care, were retrieved from the electronic patient files. Malnutrition was defined as: BMI <20 or <22 (<70 or ≥70 years), and/or >5% weight loss during EBRT, and/or >10% weight loss during follow up (compared to baseline). Overall survival was analysed using the Kaplan Meier method. Cox proportional hazard regression analyses were used to estimate Hazard Ratios (HR) for key prognostic factors.
Results
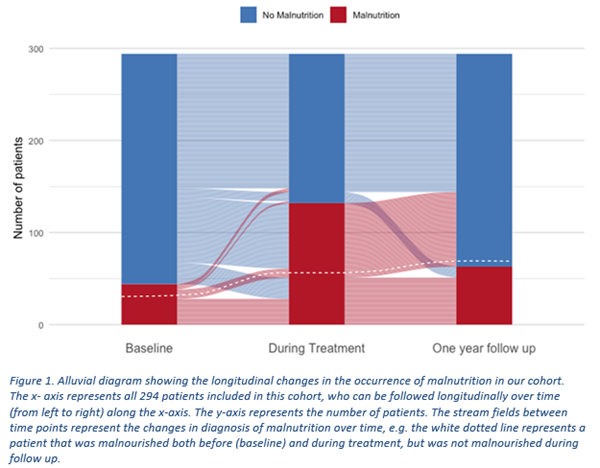
A total of 294 patients were included with a median age of 52 years at diagnosis and a median follow up of 40 months. At start or during treatment, 138 patients (47%) were malnourished (Figure 1). Of these, a substantial part (45%) were not referred to a dietician. Characteristics regarding age, smoking, histology, nodal stage and chemotherapy were balanced between patients with and without malnutrition. However, more patients with malnutrition had FIGO stage III (24% vs. 13% in patients without malnutrition). Malnutrition before, during or after treatment was significantly associated with worse survival after adjusting for age, performance score, diabetes, histology, FIGO stage, and nodal stage (3-year overall survival in patients with malnutrition was 77% [95% confidence interval 70-85] and without malnutrition 89% [95% CI 83-95]; p = 0.001) (Figure 2). Independent significant risk factors for worse overall survival were malnutrition (HR 2.17 [95% CI 1.24-3.78]), age ˃52 years (HR 2.47 [95% CI 1.43-4.24]), adeno(squamous) carcinoma (vs. squamous cell carcinoma; HR 2.24 [95% CI 1.29-3.89]), FIGO III/IV (vs. FIGO I/II; HR 2.14 [95% CI 1.22-3.75]) and N1 (vs. N0; HR 2.64 [1.48-4.70]).
Conclusion
Malnutrition is common in cervical cancer patients treated with radiotherapy and is associated with shorter overall survival. Since only 55% of the patients with malnutrition before or during treatment had been referred to a dietician, this seems unrecognised. The appropriate management of malnourished patients treated with pelvic radiotherapy requires greater awareness of weight loss and better adherence to malnutrition guidelines.