Understanding the utility of artificial intelligence in radiation oncology
Subrata Roy, B.Sc RT(T), Department of Radiation Oncology, Hcg-Ics
Khubchandani Cancer Centre, Colaba, Mumbai, India
Artificial Intelligence Background:
Artificial intelligence (AI) is a way to make software “think” intelligently in a similar manner to how intelligent humans think. AI is established through the constant study of how the human brain thinks and how humans learn and make decisions. AI mimics these activities through the application of data and high-level mathematical functions. AI is currently being introduced in various domains of the radiotherapy treatment process. The use of machine-learning models will enable the automation and optimisation of various applications to improve the treatment processes used in radiation oncology and to reduce the rates of incidence of human-induced errors.
Radiation oncology has advanced over many years from its inception with the invention of X-rays to the use of stereotactic, ionising and multi-modal treatment techniques. It is delivered by highly trained, multidisciplinary teams that comprise radiation oncologists, medical physicists and radiation therapists who work together to fulfil one goal: the precise and accurate delivery of radiotherapy to people with cancer. AI has been developed for use in various clinical setups, in which it shows a clear impact on future applications of radiation oncology.
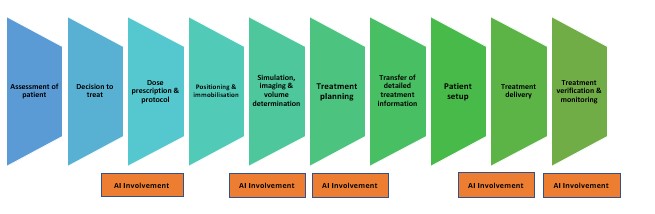
Fig 1 Stages of radiotherapy treatment at which AI may be involved
As shown in Figure 1, the radiation therapy workflow consists of various time-consuming steps, the successful completion of which has a direct impact on treatment quality and patient outcome. If the decision-making involved in these steps is machine-learned and performed by a supervised AI system, the workflow can be standardised and improved because efficiency is optimised. Therefore, radiation therapists can deliver the required dose accurately and in the most skilled manner, because they are freed up to spend more time on patient care. They can focus on their essential role of ensuring patient safety through the prevention of dose mismatching, ensuring quality control, troubleshooting and equipment supervision.
Most of the tasks that can be performed by AI machines involve the use of correctly delineated pre-treatment images to deliver precise doses. However, prediction, recommendation and action are different, and radiation therapists have a great responsibility to ensure that the AI works correctly so that doses are correct and delivered accurately. They must perform many steps that AI tools cannot recognise or fulfil. The roles of the radiotherapy healthcare professionals must be clear and organised to help to train the AI equipment, while the staff take the opportunities offered by the reduced burden afforded by AI automation to enhance their contact time with patients.
How will the use of AI transform the role of the radiation therapist?
Fig 2 Challenges afforded by use of AI in delivery of radiotherapy treatment
Radiation therapists play major roles in the verification of pre-treatment images, the use of adaptive radiotherapy and treatment delivery. The use of AI can speed up treatment delivery through the application of various data probability inputs, and the consequent reduction in the occurrence of gross errors can help therapists to gain the confidence of patients. However, to ensure the successful application of AI in radiation therapy, therapists must become familiar with its applications and the uses of different tools associated with the workflow to improvise the existing workflow. Also, while advances in technology bring AI closer to reality than it was previously, resolution of the practical, ethical and legal issues that surround AI implementation remains in its infancy. Efforts are underway to define the degree to which the use of AI must be validated and how much experience in AI use is required before it can take control of existing technologies and clinical tools. Currently, in many cases, a supervising radiation therapist must review all the steps the AI has performed before the treatment is conducted. Radiation therapists retain the role of monitor and decision-maker.
Challenges of implementation and feasibility of use
In many ways, radiation therapy is leading AI advances in oncology, because it is useful to fuse imaging modalities and to remove treatment-delivery bias, and because the ongoing development of AI deep-learning methods is poised to facilitate clinical decision support, automated image-guided adaptive therapy, and the matching of live images with projected doses.
AI is different from previous advances; despite the technology’s capabilities, the information contained in a machine-learning system is never complete or comprehensive. A machine can make decisions only when the programming reaches a tipping point at which it makes sense to confirm or deny the queried information. So, although AI equipment might be able to analyse a lot of information more rapidly than a human can, the machine requires a therapist’s approval of the decisions made and the therapist’s ability to make judgment calls regarding the administration of the treatment.
Discussion
The current and potential effects on patient care of the use of AI are indisputable. AI technologies are proving helpful in patient care as they can be used to analyse data that facilitates improved public and individual health. Analysis of more data can support digital health systems and provide positive patient experiences. The use of AI is a logical step in the continued improvement of medical devices that radiotherapy professionals use. Public awareness of the advantages of the use of AI and machine learning should be increased and transparency should be ensured regarding the use of technology with patients.
There are several areas in which AI can play roles, such as autonomous decision systems and their applications in radiotherapy, radiomics for radiotherapy of malignant brain tumours, future applications of medical physics in radiotherapy, image-guided radiotherapy for target localisation and during treatment, motion tracking in radiotherapy and driven planning systems for evaluation of online adaptive radiotherapy. Radiation therapists should lead efforts to maintain the quality of AI-based devices and to incorporate AI into quality programmes, particularly to ensure precise and accurate delivery of radiation doses to patients. Radiation therapists must be ready to change their roles and those of their colleagues to improve the health and well-being of patients.

Subrata Roy B.Sc R.T.(T)
Hcg-Ics Khubchandani Cancer Centre
Mumbai, India
References
1. What We Talk about When We Talk about Artificial Intelligence in Radiation Oncology.
Cuccia F, Carruba G, Ferrera G.J. Pers Med. 2022 Nov 3;12(11):1834.
2. Learning the Treatment Process in Radiotherapy Using an Artificial Intelligence-Assisted
Chatbot: Development Study. Rebelo N, Sanders L, Li K, Chow JCL. JMIR Form Res. 2022 Dec
2;6(12):e39443. doi: 10.2196/39443.PMID: 36327383 Free PMC article.
3. Treatment-integrated imaging, radiomics, and personalised radiotherapy: the future is at
hand.
Malicki J, Piotrowski T, Guedea F, Krengli M. Rep Practical Oncol Radiotherapy 2022 Sep
19;27(4):734-743. doi: 10.5603/RPOR.a2022.0071. e Collection 2022.PMID: 36196410 Free PMC
article.