Patient Safety Measures in Radiotherapy Practice in Radiation Oncology - PDF Version

Radiation therapy is one of the most important options for the treatment of cancer. According to available best practices [1], 52% of patients should receive radiotherapy at least once during the treatment of their cancer. Along with other modalities such as surgery and chemotherapy, it plays an important role in the treatment of 40% of patients who have had their cancer cured [2]. Radiation therapy is also a very effective treatment option to alleviate advanced or recurrent cancer and manage symptoms. Radiation therapy treatment is a multi-step, complex process and professionals who deliver it must have an understanding of radiation safety, physics and biology, clinical oncology, dosimetry, radiotherapy planning, patient simulation and immobilisation, and how it interacts with other therapies.
In India, as in other countries, the main health professionals who are involved in the delivery of radiation treatment are radiation oncologists, radiation therapists (RTTs), medical physicists, oncology nurses, treatment coordinators and dieticians. Representatives of each of these groups work through an integrated process to plan and deliver radiation therapy to patients. The main stages of the radiotherapy treatment process of care have been agreed upon by the radiotherapy safety expert consensus group of the World Alliance for Patient Safety [Figure 1].
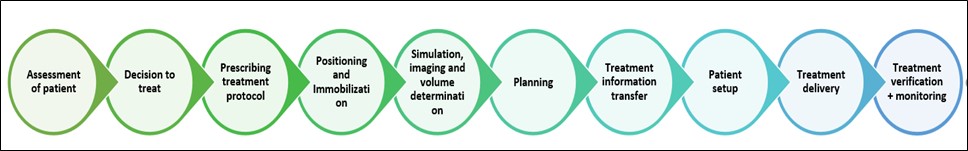
Figure 1: Stages of the radiotherapy treatment process
Radiation therapy is a complete patient-treatment pathway with many links in the chain, so the chances of error are high. The modern radiotherapy department is multi-system dependent and it relies heavily on the transfer of patient data between different units, systems, and staff in different disciplines.
Similarly, the rapid development of new technology enables the creation of complex treatment plans for many patients individually [3], but increased treatment complexity and patient throughput create an environment in which treatment incidents are more likely to occur. The development of a comprehensive quality assurance (QA) system that includes clear and uniform implementation protocols and timely assessment of error rates can reduce the rates of incidence of accidents.
Daily practices followed in India for patient safety in radiation oncology
In India, we follow a careful safety protocol, the steps of which are listed here:
- Daily check of patient’s name, verified through the use of photo ID. The patient’s photo is acquired during simulation and attached to the hospital ID number in the database.
- Selection of the appropriate imaging protocol enables the acquisition of optimum quality images at the least possible radiation dose to the patient.
- All the treatment-related parameters for a patient that are decided during the simulation step, such as patient orientation, set-up instructions, set-up photos and reference points are saved in the database. These details are checked during treatment to ensure the correct treatment is given.
- Avoid patient falls. Check the treatment table daily to avoid error.
- Document patient information on falls or occasions when a fall is narrowly averted and transfer to the database.
- Always assist the patient to climb onto the treatment table and to lie down before the table is raised.
- Monitor patient through the use of CCTV during treatment delivery.
- Always use patient safety and support items. Ensure that the audio system is working during the morning QA checks and the stages of treatment.
Through the use of an effective error management system and the tracking of the progress of error reduction along the learning curve, the occurrence of errors is minimised as much as possible and consistent with accumulated experience. The use of patient safety systems has led to the development of a risk profile that is useful to identify high-risk practices in radiation therapy and targeted interventions. We strive to reduce risk and to improve the safety of patients. To improve the quality of life of patients, the medical system must always place patient safety and care first and adhere to the mantra, “health workers and patients: safer and better together”.
.jpg.aspx)
Prakash Umbarkar
Sr. radiation therapist
P.D Hinduja Hospital
Mumbai, India; and
National academic coordinator & West zonal secretary
Association of Radiation Therapy Technologists of India (ARTTI)
Grievances &activity incharge, ARTTI
Email: umbarkarprakash@gmail.com
References:
- Delaney G et al. The role of radiotherapy in cancer treatment: Estimating optimal utilization from a review of evidence-based clinical guidelines. Cancer, 2005, 104:1129-1137.
- The Swedish Council on Technology Assessment in Health Care (SBU). Systematic Overview of Radiotherapy for Cancer including a Prospective Survey of Radiotherapy Practice in Sweden 2001 – Summary and Conclusions. Acta Oncological, 2003, 42:357-365.
- Huang G et al. Error in the delivery of radiation therapy: results of a quality assurance review. International Journal of Radiation Oncology Biology Physics, 2005, 61(5):1590-1595.