Clinical application of linear accelerator in stereotactic radiotherapy - PDF Version
Stereotactic single-dose radiosurgery (SRS) is an effective technique for the irradiation of brain tumours. A high dose of radiation is delivered in a single treatment fraction to a small intracranial volume while normal, healthy structures are spared irradiation. Stereotactic radiotherapy (SRT) is a non-invasive radiotherapy technique that can be used to deliver a high dose of radiation in multiple treatment fractions to a target volume while saving normal structures [1]. This method is known as fractionated stereotactic radiotherapy (FSRT). The goal is to capture the target volume in a high radiation dose and use a steep dose gradient to spare the surrounding normal tissue.
Hypofractionated radiotherapy enables the delivery of high doses of radiation per fraction while minimising adverse effects, all while maintaining good local tumour control. SRT is increasingly becoming the preferred treatment for intracranial metastatic lesions, as well as for brain tumours of up to 3cm in size, not only because of its efficacy in providing good local control, but also because of its limited long-term toxicity, especially in terms of neurocognitive function [2].
SRT at the Clinical Center of the University of Sarajevo (KCUS) has been conducted since March 2019, via both SRS and FSRT. Most of the patients who are treated with the SRT technique are those with intracranial metastases as well as a few patients with benign tumours. In addition to the treatment of brain tumours, stereotactic treatment has been successfully applied to treat metastatic lymph nodes in the abdominal and pelvic regions.
SRS / FSRT of brain tumours
All patients in whom stereotactic treatment of brain tumours was indicated were irradiated with the RapidArc technique, on the linear accelerator TrueBeam (Varian (Palo Alto, US)) with a photon energy of 6MV, flattening filter-free (FFF). Image-guided radiotherapy (IGRT) was applied to verify patient position and geometric precision was investigated using on-board imaging kV-imaging systems, cone-beam computed tomography (CBCT) and Kv-kv pair imaging.
The first patient treated with the FSRT technique for metastatic brain cancer was admitted to the radiotherapy centre at the end of March 2019.
This paper describes a retrospective analysis of data from March 2019 to May 2021, which included 35 patients who were treated with SRT. Most of the 35 patients had been diagnosed with metastatic brain tumours (28), for which stereotactic treatment was indicated. In addition to metastatic changes, patients with vestibular Schwannoma (4), trigeminal neuralgia (1), recurrent meningioma (1) and cerebral pinealocytes (1) were treated with the stereotactic technique (Figure 1).
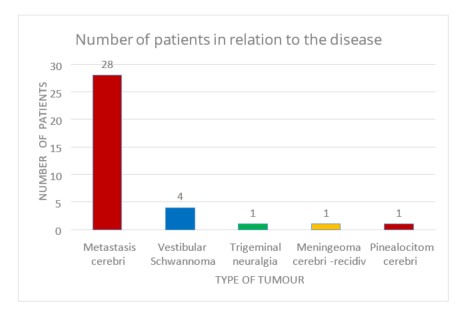
Figure 1. The numbers of patients in relation to the types of tumour treated
Among the 28 patients who showed metastatic changes in the brain, the most common treatment regimen (which was used for 15 patients) consisted of a single-fraction at a delivered dose of 18Gy, though a few patients received different doses. Seven patients were treated through a five-fraction regimen with a dose of 20Gy, and six patients received a three-fraction regimen, the most commonly delivered dose of which was 21Gy (Figure 2).
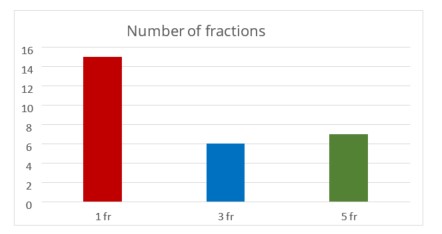
Figure 2. Numbers of patients with metastatic tumours who received the most frequently used fractionation regimens
Most of the patients who were treated for brain metastases received a single dose of 18Gy in a single-fraction regimen of planned treatment dose (Figure 3).
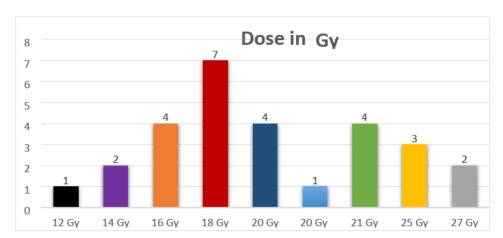
Figure 3. Prescribed radiation doses in relation to the numbers of patients treated for brain metastases
Table 1 shows the fractionation regimens and total doses that were used to treat brain tumours other than metastatic lesions
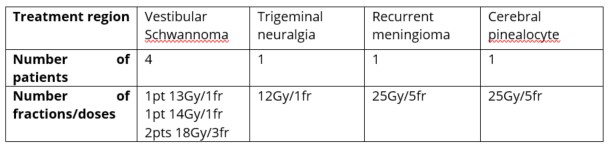
Table 1. Radiation dose and fractionation for treatment of other brain tumours through the SRT technique
Immobilisation of the patient for SRS treatment
At the KCUS, the patients are positioned and immobilised for SRS treatment through application of the trUpoint ARCH system (CIVCO Radiotherapy) (Figures 4 and 5).

Figure 4. The trUpoint ARCH system for SRS Figure 5. Positioning and immobilisation of the patient using the trUpointARCH system
Treatment planning
Treatment for SRS treatment is planned through use of the Eclipse planning system (Varian). The target volume and organs at risk are defined and contoured through use of an imaging CT simulator for planning (Canon Aquillion LB) and fusion with magnetic resonance images (MRI). The radiotherapy plan is verified and quality is assured on the linear accelerator through use of a Matrixx Evolution phantom (IBA Dosimetry) in which the deviations must not exceed 2mm and 2%, gamma pass
IGRT for stereotactic treatment
The patient's position and the geometric precision of the treatment during the procedure are verified by use of CBCT images.
The patient is positioned in an identical position to that used on the CT simulator, following the set-up sheet and reference markers on the patient mask. According to the plan and defined displacements, a delta couch shift is performed, followed by a CBCT verification (Figure 6).
.jpg.aspx)
Figure 6. Pre-treatment verification of patient position and target using CBCT
Geometric deviations in translational movements of up to 2mm, as well as pitch and roll of up to 20, are aligned with the patient's treatment table, after satisfactory online verification of the target volume. Images are matched based on bone anatomical structures and online visualisation and verification of the target volume. Auto matching is limited to within 2mm according to the target volume on CBCT images that are reconstructed per 1mm thickness. In case of larger deviations from the above, the patient's position is re-checked and corrected, in consultation with a radiation oncologist. Prior to the delivery of the prescribed dose, images are taken of the patient at each table rotation according to the position in the plan. A control CBCT is taken at the end of the treatment to check for possible intrafractional movements. These are dependent on the patient's general condition and cooperation during treatment delivery. The pre- and post-treatment CBCT images are compared. Figure 7 shows slight submillimetre deviations that may be observed.
.jpg.aspx)
Figure 7. Deviations between pre- and post-treatment positions of patient shown by CBCT imaging
This method of verification of the position of the patient and the target helped to establish and prove the validity and accuracy of the trUpoint ARCH immobilisation system for SRS treatments of brain tumours.
Based on the positive outcomes that were observed in most patients who were treated with SRT, treatment of patients with multiple brain metastases has recently begun. During 2021, five patients with multiple intracranial metastases were irradiated during the same day (Figure 8).
.jpg.aspx)
Figure 8. Pre-treatment CBCT of a patient with multiple metastatic lesions
The total dose that was planned for each individual lesion was 12Gy. A plan with a defined treatment isocentre was drawn up for each metastatic lesion.
Patients tolerated the treatment well, with no acute adverse reactions.
The results so far indicate that good therapeutic local disease control was achieved in the first patients irradiated with the stereotactic technique. These effects were measured in terms of complete eradication or reduction of metastatic changes. Longer follow-up is required to assess late toxicity, final clinical outcome and eventual recurrence of the disease.
Hypofractionated stereotactic radiotherapy of the lymph nodes of the abdomen and pelvis
During 2021, four patients were treated with the SRT technique for oligometastatic lymph nodes in the abdomen and pelvis. Patients were treated with the RapidArc technique on the TrueBeam linear accelerator, with a radiation energy of 6MV FFF. The prescribed total dose was 25Gy to 30Gy delivered in five treatment fractions.
The patient was positioned and immobilised through use of the base plate for the abdomen and the kneefix and feetfix aids to position the lower extremities. A vac lock or thermoplastic mask was applied for additional immobilisation of the patient. Reference marks were marked on the immobiliser and tattooed on the patient.
The patient's position was verified by use of CBCT imaging before treatment (Figure 9).
.jpg.aspx)
Figure 9. Pre-treatment CBCT presentation of abdominal lymph node treated with stereotactic technique
Preliminary results showed that use of SRT for abdominal and pelvic lymph node metastases was feasible with good clinical results in terms of a high rate of local disease control and toxicity rates. Even though most patients eventually show progressive disease elsewhere, the local control that can be achieved through use of SRT is potentially significant for the maintenance of quality of life and to delay the need for further chemotherapy. Based on the evidence and results so far, the SRT technique will soon be applied in our centre to the lung and liver regions.
Conclusion
Based on follow-up and evaluation of MRI controls at least six weeks after treatment, patients treated through application of the SRT technique enjoyed good outcomes and significant effects of therapy in terms of eradication of metastatic lesions and benign changes in the head region. Also, a remarkable effect has been demonstrated of hypofractionated SRT on pathologically altered lymph nodes. To observe a longer-lasting therapeutic effect, follow-up of the patients occurred over a prolonged period.
Enis Tinjak, medical radiology technologist, and Velda Smajlbegović, MD, PhD
Clinical Center, University of Sarajevo
Sarajevo, Bosnia and Herzegovina

Enis Tinjak
E-mail: t-enis@hotmail.com

Velda Smajlbegović
E-mail: veldasmajl@hotmail.com
References:
Kim Y-J, Cho KH, Kim J-Y, Lim YK, Min HS, Lee SH, et al. Single-Dose Versus Fractionated Stereotactic Radiotherapy for Brain Metastases. International Journal of Radiation Oncology*Biology*Physics. 2011 Oct;81(2):483–9.
Dumont Lecomte D, Lequesne J, Geffrelot J, Lesueur P, Barraux V, Loiseau C, et al. Hypofractionated stereotactic radiotherapy for challenging brain metastases using 36 Gy in six fractions. Cancer/Radiothérapie. 2019 Dec;23(8):860-6.