Expanding Global Access to Radiotherapy – pragmatic steps for consideration in providing cancer care in sub-Saharan Africa - PDF Version
Equity in global access to radiotherapy continues to be a pertinent topic within the oncology community. According to data that are available on the website of the Directory of Radiotherapy Centres that is part of the International Atomic Energy Agency (IAEA), 70% of countries that are without a single radiotherapy machine are in sub-Saharan Africa.
Zambia, a lower middle-income country in the south central part of sub-Saharan Africa, is fortunate to have overcome the first step to achieving access to radiotherapy by establishing its first comprehensive cancer centre in 2006. This was set up in collaboration with international partners such as IAEA and the Organisation of Petroleum Exporting Countries’ Fund for International Development (OFID). Many milestones have been achieved, as has been highlighted in a previously published profile by the director of cancer control at the local Ministry of Health. Achievements include the establishment of a training programme for human resources, development and implementation of the first national cancer control strategic plan, expansion of the cancer centre services to include in-patient facilities and the introduction of advanced brachytherapy techniques. However, many more milestones need to be gained before a plateau is reached in the figures for morbidity and mortality and the commencement of a descent for the numbers of the most preventable and curable cancers.
At this year’s Canadian Association of Radiation Oncology (CARO) global oncology symposium, which was co-hosted with Canadian and European colleagues from the European SocieTy for Radiotherapy and Oncology (ESTRO), enquiries were made about what further efforts were needed in Africa. This collaborative approach by which more developed nations assist the less developed is particularly important as it enables the prudent use of resources by avoidance of repetition of mistakes (learning from those who have done it) and the employment of best practice adapted to the local environment (tapping into local experts). This method should lead to an improvement in quality of care for cancer patients in many places around the world. This article provides some answers to this question.
A good starting point would be to recognise the heterogeneous needs across the sub-Saharan African region in terms of radiotherapy. Twenty-nine (out of 54) African countries have 255 radiotherapy centres, which are concentrated in the most northern (136) and southern (60) parts of the continent. The other 26 countries do not have any radiotherapy centres.
Establishment of radiotherapy centres has taught us that the capital cost of the projects is not the greatest problem in the grand scheme of things. The maintenance of infrastructure and retention of staff must be recognised as bigger threats. Health systems that have weak quality assurance programmes and place cancer control as a low priority in terms of national budget allocations must be supplied with good service contracts when radiotherapy is being introduced into a country. Without this, the physical presence of machines will not equate to access to care, because the machines will break down and their repair or replacement takes a long time. The continuous peddling of second-hand machines, the spare parts of which sooner rather than later go out of production, is not an equitable approach as a global community and should be discouraged. Partners with stronger voices than those in Africa must advocate against this rather than see the developing nations as a dumping ground for unwanted equipment. Advocacy for setting minimum standards for the sale of radiotherapy units must be seen as facilitation for the basic human rights of people in vulnerable countries that have under-developed systems. From a public health perspective, in developing nations the investment in new radiotherapy machines competes poorly in terms of priority compared with infectious disease and maternal and child health programmes, which may receive precedence as indicators of reaching sustainable development goals. Therefore, opportunities to spend on radiotherapy must be used well.
The 2015 Lancet Commission on expansion of global access to radiotherapy showed that 55,800 radiation oncologists, medical physicists and radiotherapy technicians would be needed in low and middle-income countries (LMICs) to supply sufficient radiotherapy coverage to meet demand. This will not be attained due to the continuous brain drain that is not only due to financial gain but unsustainable working conditions that affect the mental health of these professionals. Innovative and deliberate initiatives need to be introduced to address this important aspect that is often overlooked as employers rely instead on a sense of patriotism on the part of the health-care professionals. A career progression path for staff and provision for growth in the systems of employment in the countries must be laid out clearly.
In relation to the above two points, increased investment in leadership and governance of radiotherapy programmes must be established that follows global standards. High-level policy makers and technocrats need to work in a multidisciplinary manner. Programmes fail or they are unsustainable due to a ‘copy and paste’ system that is transferred from developed countries to LMICs. A robust, scientific, individual country approach with maximal engagement of local technocrats is vital to find solutions rather than to tick the sustainable development goal boxes.
Bishal Gyawali, a medical oncologist and scientist at Queen’s University Cancer Research Institute in Kingston, Ontario, Canada made a compelling presentation at the American Society for Radiation Oncology (ASTRO) annual meeting this year. He spoke about meaningful contribution to global oncology through development of treatments in LMICs. I quote:
- Donate – donate what they need, not what you don’t need;
- Mentor – teach what they need, not what you want to teach;
- Teach how to fish, do not provide them with fish. The hallmark of an excellent teacher is that her trainees become independent;
- Provide funds/grants and protect time for research;
- Invite and give opportunity;
- Collaborate on research and trials that are relevant to the LIMIC setting;
- Institute bidirectional learning.
It is an exciting and promising time to be in the cancer control field and, in particular, in radiotherapy. The World Health Organisation (WHO) has launched a global strategy to accelerate the elimination of cervical cancer. The WHO has also called for childhood cancer mortalities to be reduced in LMICs. Radiotherapy forms an important part of the armamentarium to deal with these important issues. A holistic and evidence-based approach must be taken if we are to achieve ambitious goals.
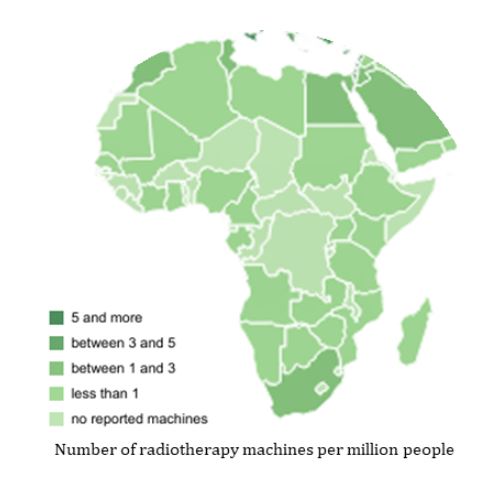
Data source IAEA Directory of Radiotherapy Centres: www.dirac.iaea.org

Leveraging international support for pragmatic steps that are needed to expand global access to radiotherapy

Dorothy Lombe
Clinical and radiation oncologist
Cancer Diseases Hospital
Lusaka, Zambia